This is Naked Capitalism fundraising week. 623 donors have already invested in our efforts to combat corruption and predatory conduct, particularly in the financial realm. Please join us and participate via our donation page, which shows how to give via check, credit card, debit card, or PayPal. Read about why we’re doing this fundraiser, what we’ve accomplished in the last year, and our third goal, well-deserved bonuses for our guest writers.
By Lambert Strether of Corrente.
Readers will recall that we summarized the effects of the Centers for Medicare & Medicaid Services (CMS) proposed new MACRA rules here:
Crapifying Medicare with the New MACRA Program
MACRA’s goal is to revise how doctors are paid for Medicare by incentivizing for “quality,” replacing the current, fee-for-service system. To that end, HHS proposed to introduce two new payment systems: the Merit-based Incentive Payment System (MIPS), and Alternative Payment Models (APMs). Most doctors would automatically qualify to be a part of MIPS. The difficulties:
MIPS Cannot Measure What MACRA Purports to Incentivize
MIPS really does propose “to provide each physician with a composite score between one and 100” for each individual doctor [and then use that score to structure incentives]. But as PNHP’s Kip Sullivant writes,] with the exception of a few services, measuring cost and quality accurately at the individual doctor level is not possible.
And:
APMs are Handwaving
- MACRA does not describe the entities that will qualify as APMs;
- MACRA sets standards for these entities that cannot be met by the vast majority of conceivable entities, including today’s most faddish APMs – ACOs and “medical homes”;
- MACRA says APMs must expose doctors to “risk above a nominal level,” but doesn’t say what “nominal” means; and
- MACRA says doctors who join APMs will earn a 5 percent bonus on revenues received through APMs, but the law fails to define “revenue” (options include revenue from Part A, Part B, Part D, all or some of those parts, or revenue received for particular services).
Among many other problems.
Well, HHS was now taken public comments into account and issued the final MACRA rule. Sadly, MACRA remains broken. But first let’s see what HHS did. Becker’s Hospital Review has a very good summary of the changes between the proposed and final rules:
After a listening tour and nearly 4,000 public comments, CMS released the final rule Friday for the Medicare Access and CHIP Reauthorization Act [MACRA], a landmark payment system for Medicare physician fees that replaces the Sustainable Growth Rate formula.
(Nobody’s arguing that the Sustainable Growth Rate formula wasn’t broken; it created a large administrative burden and led to payment cuts for physicans. Still, it’s always possible to make things worse, or bad in new ways!) Here is the official view:
“It’s time to modernize the Medicare physician payment system to be more streamlined and effective at supporting high-quality patient care. To be successful, we must put patients and clinicians at the center of the Quality Payment Program,” CMS Acting Administrator Andy Slavitt said in a statement. “A critical feature of the program will be implementing these changes at a pace and with options that clinicians choose. Today’s policies are designed to get all eligible clinicians to participate in the program, so they are set up for successful care delivery as the program matures.”
(Note the assumption that we can, in fact, measure quality.) Here’s what Slavitt[1] means by “at a pace and with options” (again from Becker’s Hospital Review). For MIPS:
Since CMS rolled out the proposed MACRA rule, it has settled on a gradual ramp to full participation, allowing physicians to pick their pace between the following four options in 2017.
- No participation and an automatic 4 percent negative payment adjustment.
- Submission of a minimum amount of data — i.e. one quality measure — and a neutral payment adjustment.
- Submission of 90 days of data for a potential small positive payment adjustment or a neutral adjustment.
- Submission of a full year of data for the potential to earn a moderate positive payment adjustment.
And for APMs:
The final rule firms up details on what programs will qualify as advanced APMs. First, to qualify, advanced APMs must meet three requirements: Use certified EHR technology, base payments on quality measures comparable to MIPS and require providers to bear more than nominal risk.
If you compare this summary to “APMs are Handwaving,” above, you’ll see that, if Becker is correct, only the first item has been addressed.
Summarizing, then: CMS has backed off on draconian measures to force physicians into MIPS pronto, and has addresed one, but not all, of the implementation problems with APMs. (Here is an online tool from the AMA that helps physicians figure out where they fit within these programs. I set up an account and tried the tool, and it reminded me a lot of all those ObamaCare calculators that turned out to have very little to do with how the Exchanges turned out to work, or not work. Your mileage may vary!)
Before turning to the effect of MACRA on rural areas specifically, let’s look at a general indictment of the program. Remember the “composite scoring” concept? The crazypants meritocratic scheme no doubt well-intentioned effort to measure quality by assigning a “grade” to each individual physician? Niam Yaraghi in Health Affairs Blog gets into the weeds on how the scoring will be done:
MACRA Proposed Rule Creates More Problems Than It Solves
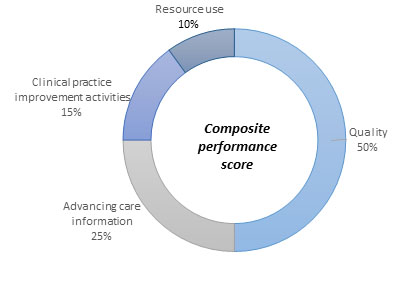
[MIPS] assigns a “composite performance score” for each clinician based on four domains of quality, advancing care information, clinical practice improvement activities, and resource use as shown in Figure 1. [shown here]
To calculate this score, only the resource use element is directly measured by the Centers for Medicare and Medicaid Services (CMS) based on submitted Medicare claims, and the other three elements are self-reported by clinicians. In 2019, clinicians who outperform their peers will receive a 4 percent bonus while those who don’t, will face a 4 percent penalty. The bonuses and penalties rise to 5 percent, 7 percent, and 9 percent in the subsequent three years.
Oh. My. God. Self-reporting with financial incentives for “good reports.” CMS just incentivized accounting control fraud at the doctor’s office level. And they just turned the Medicare payment system into a phishing equilibrium. Yaraghi continues:
Along with my colleagues, I have conducted empirical studies which confirm The New York Times’ anecdotal evidence, showing that about 12 percent of nursing homes highly inflate their self-reported measures as a strategy to increase their overall star rating. Note that such manipulations take place even without powerful, direct financial incentives. Compared to nursing homes, clinicians[2] will have significantly stronger financial incentives to exaggerate their self-reported measures, rendering the system ineffective.
And then there’s the problem of not knowing what “quality” means. Yaraghi goes on:
An Unreliable Quality Score
The six measures for the quality domain are chosen by physicians from a wide variety of available measures depending on their specialty and preferences. For example, a family physician could choose six measures from the 38 available options.
This means that there will be 2,760,681 possible combinations of quality profiles reported by family physicians alone. Each of those possible profiles measures a different aspect of medical quality. This large variation makes it impossible to evaluate physicians and assign a reliable performance score to them. Scoring physicians of identical medical specialty based on different measures is akin to comparing students’ performance based on different types of questions and exams.
Oh dear. Yaraghi concludes:
While HHS had the best intentions in creating MIPS, the proposed rules are so abundant with flaws and weaknesses that it is very difficult to imagine the program could ever be successfully implemented.
But they’re going ahead with it anyhow, aren’t they?
Having looked at a general indictment of MACRA, let’s look at MACRA’s effect on rural practitioners. At the outset, let’s note that some of the changes between the proposed and final rules were designed to ease their burden:
The number of measures that must be reported in other categories have been reduced, especially for small and rural providers.
Providers must report up to six quality measures, including one outcome measure, and must attest [self-report] to having completed four improvement activities.
And this is meant to reassure:
“In creating a clear path for small, independent physicians to embrace the transition to value, CMS makes it possible for leading independent practices to reduce costs, boost outcomes and thrive,” said Dr. Farzad Mostashari, former National Coordinator for Health IT who is now chief executive at Aledade.
(Fine example of the revolving door there, eh Farzad?) Note that the “transition to value” is codswallop, (a) because MIPS self-reporting incentivizes fraud and (b) the quality scores are a steaming load of incommensurate crapola. It’s hard to imagine any physician with a functioning bullshit detector (“embrace the transition to value,” “boost outcomes,” “thrive” pin my bogometer) reading Mostashari and not throwing up a little in their mouth.
So, Dr. Jean Antonucci is not re-assured. From HealthCare Finance:
For small practices like those run by Jean Antonucci in Farmington, Maine, succeeding under new MACRA regulations will all boil down to the details. Unfortunately with MACRA, there are just so many she is just one of the many small practitioners dreading the rollout. That’s not surprising given the 4,000-plus comments the Centers for Medicare and Medicaid Services received on the law.
“I don’t gain anything positive from this that is not financial, and the financial gain is so tiny for the enormous complexity and reporting burden. It’s not simple and it’s not useful,” Antonucci said.
Nor is Dr. Lee Gross:
Lee Gross, MD, a primary care physician in a CMS-designated underserved area for primary care in southern Sarasota County, Florida, said his staff includes two physicians and one nurse practitioner. He lists his group as the last independently owned primary care practice in the region.
“It’s just mind blowing how many resources we spend on just compliance,” Gross said. “We don’t have a compliance officer. Who in my practice is responsible for reviewing the legislation and making sure they are doing things right?” Gross said.
Take heart, Dr. Gross. The answer is “nobody”! You can self-report!
And here is the end game (granted, from anecdotal evidence); Antonucci, also quoted in WaPo:
Could Medicare’s new doctor payment system endanger small and rural practices?
“I have no idea what I’m going to do yet,” acknowledged primary-care physician Jean Antonucci, who has a solo practice in Farmington, Maine. Half of her patients are covered by Medicare. “If I’m going to lose money, I’ll have to see what my options are.”
As will her patients if she quits or leaves. But let’s look on the bright side; they’ll get to go shopping!
My recommendation: Put all the health care experts in this country on a garbage scow, tow them far out to sea, and cut the cable. Then hire the Canadians to install their simple, rugged, and proven single payer system here.
NOTES
[1] Poking around for information on Slavitt — the never-formally-held-accountable-for-the-ObamaCare-rollout-debacle Marilyn Taverner’s successor — I found this little nugget: “Pharma industry leaders are aware of the problem with soaring drug costs and symphathize, [Slavitt] said. The solution, Slavitt said needs to include price transparency and clear explanations to patients as to why such drug costs go up.” Oh. OK. Apparently, the policy of a single payer to muscle better prices isn’t “on the table.” I wonder why?
[2] I am using “doctor” and “physician” interchangeably; Yaraghi uses “clinician.” Probably OK for a layperson, who “goes to see the doctor,” but maybe not OK in professional circles. Can a knowledgeable reader clarify?


So much work to not just increase the rate at which physicians are compensated for taking a history.
Thanks for publishing this, I don’t feel like a lone wolf or duck out here anymore. I’ve already been out there on this one, being a former healthcare developer.
The Rise of the quants, Again! This Time In US Healthcare- Taming the MACRA Beast of Quantitated Madness For A Lot of Things That Are Probably Just Not True
Added this today and this gets all of us, front running at the prescription counter to get higher co-pays out of us, and it all leads right back to the head of CMS who’s been out there for years with all the United Healthcare incest with HHS and CMS for years!. If you read the link below, you’ll be plenty pissed off indeed.
Cigna & United Healthcare Face Class Action Suits-PBM Over Charging Customers for Prescriptions, OptumRX Pharmacy Benefit Management Software-“Front Running” Consumers With Killer Algorithms at the Drug Store
Read all the links too for even more information, this is not conspiracy, it’s the real thing for those not wanting to live in virtual software worlds today. It’s a big problem with people confusing virtual and real world values! Wrote about that in 2013.
http://ducknetweb.blogspot.com/2015/06/virtual-world-values-and-real-world-we.html
I’m sorry I used the web interface but here’s the links…next time I’ll stay with the old fashion way of just putting in a link w/o being fancy my bad here.
http://ducknetweb.blogspot.com/2016/05/the-rise-of-quants-again-this-time-in.html
Here we go again. If you haven’t figured this out yet, when you buy a Cigna Health insurance policy you get a two for one with 2 insurers. Lawsuits are filed!
http://ducknetweb.blogspot.com/2016/10/cigna-united-healthcare-face-class_16.html
I’m just so happy to see someone besides me that sees the CMS nonsense as we will be losing more doctors because of this.
Thanks very much for the links. “The internet” is in fact quite silo-ed and it’s hard for people who are like-minded on policy to find each other (and Google’s crapification of search doesn’t help).
I’d really like to know more about EHRs, and especially about the classification scheme that drives them. Any suggestions?
The links above are dead MQ!
Please fix
This illustrates the quality measurement problems pretty well.
https://dinosaurmusings.wordpress.com/2016/10/04/i-am-a-terrible-doctor-and-im-proud-of-it/
this is just brilliant analysis by lambert, many thanks to all those who donated to the fundraiser to support this sort of reporting.
Everything I know about the practice of medicine I learned from M*A*S*H. Here is but one of many quotes from that tv series that’ are applicable to the ongoing effort by large health insurance companies and their fellow travelers to control independent physicians and “financialize” the practice of medicine for their own benefit while killing consideration of the single payer option politically:
Frank Burns: “I know I’m a real asset.”
Hawkeye Pierce: “You’re only off by two letters.”
Thanks for this and your other related posts, Lambert.
as a doc married to a doc we are delighted that neither of our children chose to become docs. one is a software engineer, other a writer. one is paid well, the other not at all.
lol
I believe that incent predates and efficiently encompasses incentivize as orient does orientate and normal does normalcy.
The English language is constantly changing (and thanks, in part, though I say it, to former English majors like me). I think your cases are different:
1) Normalcy — Harding’s neologism, now dead unless used for irony.
2) orientate — I never use it. I’m guessing a vile back formation from “orientation” by college administrators
By contrast:
3) incent — way too close to “incense”, I’m afraid. “In 2016, I’m totally incented, all the time.” So there’s space for incentivize (which is in fact winning).
Lambert, regarding your point 2) – “MACRA sets standards…cannot be met by majority of entities…including ‘care homes’.” Don’t worry, it won’t matter that ‘care homes’ don’t meet the standard – US Gov will pretend they do. Half the point of MACRA, in my opinion, is to shove into ‘care homes’ the Medicare recipients who have not yet been coerced (33 states). In other words, there will be no more ‘choice’ in Medicare, everyone will be in an ersatz HMO ‘care home’.
I forgot to make mention too of the incest that exists at HHS/CMS with United Healthcare/Optum. It has been there since Hillarycare days and lots of former and current executives as fellows at the Podesta Center for American Progress who still writes healthcare policy for US gov. Everyone remember, Zeke Emanuel who’s out there in the press all the time? He’s a senior fellow at the CAP and now works at a Venture Capital fund as well, is this ethical?
http://ducknetweb.blogspot.com/2016/01/zeke-emanuel-joins-venture-capital_14.html
Also remember that CMS Andy was formerly Ingenix Andy, who had a ton of lawsuits filed again him and the company, Ingenix is a subsidiary of United Healthcare. HHS Burwell gave him a pardon on all those lawsuits and the ability to go have lunch with the CEO of United Healthcare and chew the fat or healthcare policy any time he wants.
Look what I keep seeing in the OC, doctors being bought out by United Healthcare as they maintain a practice and stay in business under current conditions. Remember United Healthcare has just under 400 subsidiaries and that’s where the action takes place.
http://ducknetweb.blogspot.com/2016/08/optumcare-doctors-to-get-allscripts.html
At 68 on Medicare is it criminal with what is going on with large general practitioners owned by hospitals? Is it only large practices that are not being encouraged by policy? Who owns the regulators? Who to complain to?
At my welcome to medicare physical I did not get a pneumonia shot or Hep C test and other things required by Medicare in the beginning. I would guess they receive a flat rate for this and save by not doing it.
Now with blood Iron and other levels out of wac and bone loss I had to advocate for myself to get tests and help. I was told when the blood test showed large changes, “we do not go looking for problems”. I was not called back when the bone loss test was -2.4 or when the Iron level was 20. Not continuing tests after giving blood and levels went down dramatically with other indicators bouncing out of range or near on the CBC. No answer for why bouncing around. What a system. I was told I would be referred to specialists, after pushing for help, that the insurance company recommended. WOW will they be controlled like my G.P. owned by the hospital system.
Now at the end of the year the drug store wants to fill new prescriptions renewals that run 3 months in the beginning. Almosts 700 out of the amount to reach the donut hole. Also they say if I have medicare I can not use the discount cards and I will be required to run certain outrageously price medications through Medicare.
When going to specialists for test that are supposed to be covered and you will not pay there are facility fees, anesthesiologist fees and other fees that even if you push you can not find out the amount. It seems these fees are variable based on what they find. Like what the medication providers say it seems they collect more money from the medicare patient because it is worth more if the find a problem because it is worth more to the patient to know they have a problem that they can not afford to treat.
There is much more but to cut to the chase everything is for profits and let the patient go to hell. I heard a new doctor to the practice talking to a colleague outside the examining room saying the the patient was S.O.L. because they did not have insurance. It still haunts me as to whether it was a defence mechanism or he had no empathy for the patient. Are the human resources hiring only money driven doctors? What is going on?
Will health care be the next banking scandal with the crosses lined up in the parking lots for those that died for the money .
David do not blame the doctor. We are just doing what we are forced to do. The Doc does not get paid more anyhow.The scandal will be more with the insurance,big HMOs,and CMS.
I do not blame the Physician Assistant for what is going on.
I have seen the P.A. for 15 years and have seen the frustration grow. I think the P.A. sees more patients than the doctors in the practice and has to work untill 11 pm to finish updating the “?” or whatever is required to complete so as to keep the number of patients seen during the day in line with the salary earned. The P.A. works 80 hours a week now to keep the billing up for their salary because of the Electronic billing system.
I believe is the “non-profit” hospital (that makes a huge profit) that bought the practice years ago that demands the numbers regardless of the cost to personnel.
I have a relative who is a Pediatric Nurse Practitioner who says the system reduces the number of children she can see by 30 percent or more. I do not know what steals the time but it seems to be making life hell for medical personnel with no benefit to the patient that I can see.
Hey, David welcome to the living hell the rest of are in.
[2] I am using “doctor” and “physician” interchangeably; Yaraghi uses “clinician.” Probably OK for a layperson, who “goes to see the doctor,” but maybe not OK in professional circles. Can a knowledgeable reader clarify?
The reason Yaraghi uses “clinician” is that MACRA applies to healthcare providers beyond just physicians/doctors. It will apply to the following ‘clinicians’ who bill Medicare:
Physician
Physician assistant
Nurse practitioner
Clinical nurse specialist
Certified registered nurse anesthetist
This list will likely be expanded in future years.
Seems like self reporting is a great neo libcon way to get positive claims(as you say, control fraud), kind of a payoff to report good outcomes, but as would be normal with neo libcons they don’t want to pay more than they absolutely have to so they low ball just to be sure… and your post script…”The solution, Slavitt said needs to include price transparency and clear explanations to patients as to why such drug costs go up.” ” just needs to be highlighted once more for emphasis. apparently “you’ll get nothing and like it” is moving up the food chain to doctors. this guy is obviously one of obamas soul brothers who believes it’s all in the messaging. If you tell people how crappy it is in a resonant npr tone then they will certainly understand they are being lectured by one of their pragmatic betters and only an unreasonable person could disagree
This is timely for me, thanks, Lambert. I switched from a terrible hospital-based PC practice to a local private practice on advice from a friend. I got a first “wellness visit” which has always been covered by my Medicare. This morning, I received a $160 bill for “99203 Office visit, New Pt. Level 3”. Nothing has changed on my end. Hope this is a coding mistake, but I may have a rude surprise. I will just go back to not going to doctors again, like the bad old days of the nineties and oughts. I look forward to reading all comments also with interest.
The “new patient” charge is becoming quite common, and the amount you were charged is about the same as what I’ve seen. As best I can tell, it’s a wildly overpriced amount for entering your personal data into the office’s computers. Naturally, Medicare doesn’t pay for administrative fees, only costs related to health care. Sadly, it seems that the only way to avoid this is to see a physician within the hospital-owned network. Since your records are already in the system, they don’t charge you for data entry–which is the only thing your $160 represents.
I’ve never had that happen that it was disallowed completely. I suspect that they won’t bill Medicaid for the part Medicare won’t cover, either. I went online to search that code, and $108 of it is covered (or was). That visit covered all of the guidelines in that code:
Your follow-up research rings a bell. It’s been 3 years since I had an invoice for “new patient”, and now that you mention it, I think Medicare did pick up part of the cost, but I still had about $70 or so that I was supposed to pay out of pocket. Since the doctor turned out to be a real jerk, and I had no intention of ever seeing him again, I just didn’t pay the balance. I never received a second invoice so I guess I was lucky.
The Macra Terror!
Personally, I think being brainwashed and enslaved by giant alien crabs might be preferable to dealing with this MACRA. Trying to read the source documents was killing me and I wonder about this: “In 2019, clinicians who outperform their peers will receive a 4 percent bonus while those who don’t, will face a 4 percent penalty. The bonuses and penalties rise to 5 percent, 7 percent, and 9 percent in the subsequent three years” – Is it really going to be a relative grading as that quote seems to imply? If so doesn’t it mean that the same proportions of physicians are going to end up being punished and rewarded no matter how good they do in an absolute sense? Reminds me of HRC’s idea of a few years back suggesting below average schools be shut down.
P.S. I put an image link in the comment but its doesn’t show up when I save it. Perhaps it’s in moderation?