Lambert here: Readers may enjoy this article, but not, perhaps, for reasons the authors would have imagined….
By David M. Cutler, Otto Eckstein Professor of Applied Economics, Harvard University, Ellen Meara, Professor of Health Economics and Policy, TH Chan School of Public Health, Harvard University, and Susan T. Stewart, Research Specialist, NBER. Originally published at VoxEU.
Recent analyses suggest that pain is on the rise among working age adults in the US. Like many public health challenges, the burden of pain is unequal. This column explores why knee pain – the top joint problem in the US – differs by education. It finds that physical demands on the job and obesity each explain about one-third of the education gradient in knee pain and that there is an interaction between the two, with physical requirements on the job associated with knee pain primarily in those who are obese.
With a COVID vaccine on the horizon, what is the greatest public health challenge facing the US? The surprising answer, by many metrics, is pain. Chronic pain is one of the most frequent reasons adults seek medical care: it restricts mobility and daily activity, contributes to anxiety, depression, and dependence on opioids, increases disability, and costs over $500 billion annually in medical care costs and reduced productivity (Institute of Medicine 2011). And with half of adults reporting that they suffer from a musculoskeletal condition, chronic pain is among the most common medical conditions. Recent analyses suggest that pain is on the rise among working age adults in the US (Case et al. 2020). Like many public health challenges, the burden of pain is unequal – those with fewer years of education report more pain.
We set out to understand the experience of pain by education focusing on one important example, knee pain. We chose knee pain because of its leading role in disability – it is the top joint problem for Americans – and because clinical measures of knee anatomy permit one to measure the degree of physical injury quite well.
For people at every education level, musculoskeletal impairments stand out as the most common cause of functional limitations, such as the inability to walk a quarter mile, climb stairs, lift heavy objects, stand or sit for two hours, stoop or bend, reach, or socialise. Nearly two-thirds of people reporting such limitations in a national survey of US adults, the National Health Interview Survey, reported musculoskeletal problems as the cause. The burden caused by musculoskeletal impairments results in more claims for Social Security Disability Insurance in the US than any other health problem, accounting for 37% of new disability benefit recipients in 2018 (Social Security Administration 2019). Only mental illness comes close as a cause of disability insurance enrollment.
Nearly half of Americans (45%) in the National Health Interview Survey report that they had symptoms of joint pain, and among these adults, knees are by far the most common joint affected (62%). Figure 1 shows the percent of respondents reporting chronic knee pain (symptoms of pain, aching, or stiffness in the past 30 days that began at least three months prior) by age and education level. Two trends are notable. Even for young adults in their 30s, pain is less common comparing college graduates to those with fewer years of education. Second, while pain rises with age for all education groups, it rises more slowly among college graduates, with the greatest gap by education occurring at age 60 when roughly 30% of people in the bottom two education groups report chronic knee pain compared with 20% of college graduates.
With such large gaps by education and significant effects on function, medical costs, and productivity, it is important to understand why knee pain differs by education. In a recent paper (Cutler et al. 2020), we set out to do that.
Figure 1 Percent of adults with chronic knee pain
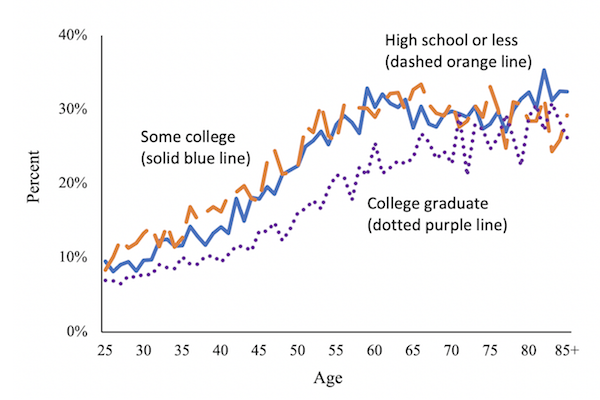
Note: Data are from the National Health Interview Survey, 2009-2016 and are weighted to be representative of the US population. Panel (a) shows symptoms of joint pain, aching, or stiffness in the past 30 days in either hip or knee, or neck or low back pain in the past three months. Panel (b) shows symptoms of joint pain, aching, or stiffness in the past 30 days that began at least three months prior.
Physical Differences in Arthritis by Education
We began by examining whether damage to the knee is greater among people with fewer years of education. The most common cause of knee pain in older adults is arthritis, a condition whose severity can be measured by x-ray. Radiologists look for space between bones, bone spurs, sclerosis (hardening or thickening of bone), and loose bodies in the knee. We examined medical professionals’ reports on knee x-rays of older Americans participating in National Health and Nutrition Examination Surveys (NHANES), a series of studies which combine interviews with physical examinations. In the NHANES, there was remarkably little difference by education in the percent of x-rays suggesting arthritis (Figure 2). The difference in knee pain by education is a result of the fact that at every level of knee arthritis – including none – people completing fewer years of education report more knee pain. We relied on data from the OsteoArthritis Initiative, a longitudinal sample of about 5,000 people with or at risk of severe arthritis and pain. Two-thirds of the educational gaps in pain remained even after controlling for additional measures of knee damage beyond x-rays, including MRI-identified cartilage damage, meniscal tears, and bone marrow lesions, and reports of crepitis (creaking).
Figure 2 Severity of knee arthritis and pain conditional on arthritis
a) Population distribution by x-ray findings
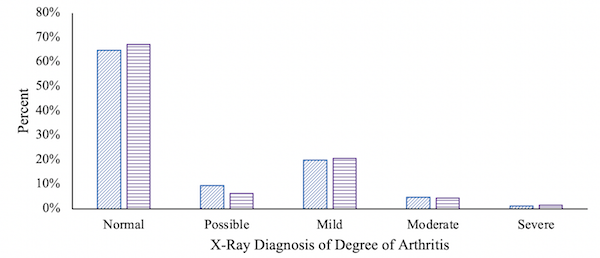
b) Precent reporting knee pain
Note: Data are from the second phase of NHANES III, 1992-94, and are weighted to be representative of the US population. The sample is people aged 60-74 with both reports of knee pain and x-ray readings. Each observation is a knee.
Excess Weight and Physical Demands on the Job
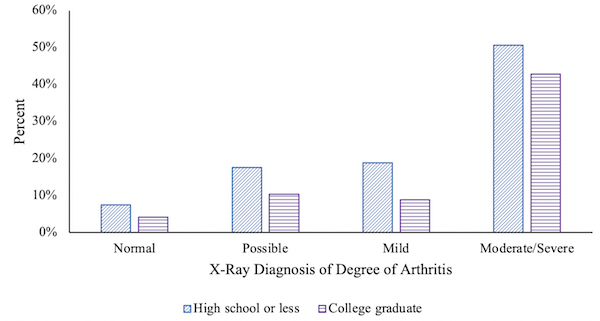
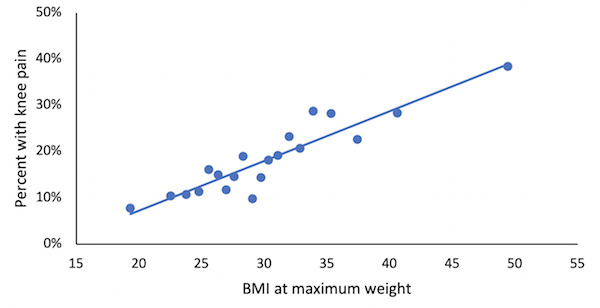
Although the gaps in the rate of knee pain by education are not explained by differences in arthritis damage, at any given level of arthritis the load placed on a knee joint could differ by education. Two phenomena that are more common in adults with fewer years of education, excess weight and repetitive stressful motion, could increase the load placed on a joint (Okifuji and Hare 2015, Vignon et al. 2006, Sokolove and Lepus 2013). Figure 3 shows how reports of pain compare with measures of a person’s highest reported body mass index (BMI – a measure of obesity based on weight and height), and compared with an index of the physical demands of their job. Reports of knee pain rise in lock step with body mass, and pain also increases with the physical demands of one’s longest occupation. After controlling for obesity (at maximum BMI) and the physical demands of one’s longest-held job, the remaining gap in knee pain by education is only 30% as large.
Figure 3 Relationship between knee pain, obesity, and job requirements
(a) BMI at maximum weight
(b) Physical requirements on longest job
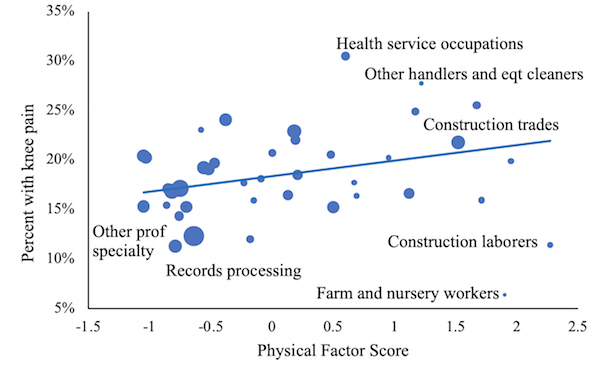
Note: Data are from the NHANES, 1999-2004, and are weighted to be representative of the US population. The sample is people aged 45-74. In panel (b), the physical factor is the first factor from a principal component model including strength requirements, reaching, climbing, and stooping. The four physical measures are: (1) a five point strength scale (sedentary, light, medium, heavy, very heavy); (2) the percent of workers engaged in climbing and/or balancing; (3) the percent engaged in stooping, kneeling, crouching, and or crawling; and (4) the percent engaged in reaching, handling, fingering, and/or feeling. Each circle is weighted by the population holding that occupation.
Psychological Factors and Pain
These remaining differences in pain could have a psychological as opposed to physical basis. For example, the same neurotransmitters in our brains influence both pain and mood (Marsala et al. 2015). Thus, it is possible for symptoms of depression to affect our experience of pain. Experimental evidence lends support to this notion, since people with depressed mood report more pain in response to the same stimuli (Nakao and Barsky 2007). We estimated how reports of pain differed by education controlling for measures of obesity, physical demands on the job, and several domains of psychological wellbeing including life satisfaction, positive and negative affect, sense of control, and psychological wellbeing. Though measures of depression were lower and psychological factors were more positive among people with more years of education, psychological variables had little relationship to knee pain.
Treatment of Musculoskeletal Pain
Of course, people with less education are less likely to have health insurance and have less contact with the medical system when they do. Thus, treatment for pain may be less helpful in reducing pain. Upon reaching age 65, the age of eligibility for Medicare benefits, the probability of having health insurance rises more than 10 percentage points for adults with a high school degree or less education, while no such change occurs for college graduates, virtually all of whom have insurance coverage before reaching age 65. So, if access to care is related to knee pain, one would expect a dramatic increase in arthritis-related doctor visits, medication, or joint-replacement surgery at this age. However, none of these healthcare outcomes changes much at age 65, suggesting there is little role for medical care as an explanation of differences in knee pain.
So, what does the evidence on knee pain by education suggest about the future? Based on forecasts of employment by the Bureau of Labor Statistics through 2026, work-related physical demands are expected to rise. This may surprise most readers, but it stems from the large projected growth in occupations like home health aides, personal care workers, janitors and cleaners, and construction laborers. Furthermore, employment in occupations with low physical demands, like secretaries, is expected to continue to decline. There are no forecasts for obesity, but against a backdrop of cheap (not necessarily nutritious) calories, obesity has been rising steadily in recent decades. In 1988-1994, the percent of adults age 45-74 obese at their maximum weight was 41%, but this figure has steadily risen (reaching 55% in 2015-16), and the prevalence of obesity continues to be higher among adults with fewer years of education. Meeting the challenge of the ongoing risk of obesity and physical demands that fall with unequal burden among those with lower education is among the most important medical and social goals for the post-COVID era.
References


So, what does the evidence on knee pain by education suggest about the future? This is funny because what it suggests regarding knee pain is when you can’t hardly move you get a joint replacement and once you do you say, “I wish I’d done this ten years ago!” Words spoken by 100% of knee replacement recipients, in my experience. Never known one not to exclaim this.
uninsured people are not likely to get a knee replacement. The question isn’t “what are the people who have been favored by government policy for the last 40 years going to do (clutches pearls)”, it’s “what are the people who’ve been completely screwed for the last 40 years going to do?”
The implicit answer is of course neoliberalism rule # 2, preferably at or before age 65 so they don’t threaten the formers social security. Not mentioned is that a computer programmer who gets knee surgery can work while recovering, construction workers not so much
Three observations from my knee replacement experience a year ago (at least in my (former) community, knee replacement patients were required to sit through a half-day orientation about the surgery and what to expect after) and further conversations with my aged mother-in-law, who is contemplating such and has had many conversations with various health personnel and contemporaries.
1. Medicare is apparently quite liberal in approving knee replacements (as in, no one rejected). My M-o-L has the typical variety of ailments for an almost 90-YO, including knee pain, and has been twice waved through for knee replacement surgery despite it being relatively far down the list of her current reported ailments, (She is, for her age, relatively healthy but has never followed through with the surgery due to other health complications arising at inconvenient moments in terms of scheduling.) In my own orientation, I was in my late 50s apparently the youngest person in a group of 20 or so.
2. I was also by far the least obese person there (my BMI is probably typical or lower than most people with knee pain who do sedentary white-collar work and were once athletic – overweight but not obese). It was both shocking and not to look at the group surrounding me, hoping for a surgical solution to what was clearly at least partly a weight issue.
3. Being now a year out from the surgery myself and talked to many others who have had it (with varying degrees of reported success), I conclude (always subject to new evidence) that a) fitter patients report more satisfaction afterward, b) most patients report some degree of pain relief, with fitter patients reporting more, and, most importantly, c) the pain relief comes 2 different ways. The first way, available to all, is that certain nerves are cut during the surgery so overall feeling in the knee is substantially less afterward. Also, the synthetic parts (various metals and silicones) obviously have no nerves in them, so that actions that would formerly cause pain now don’t, even if they involve the same movements. The second way, much more available to fit patients, is taking advantage of the first form of pain relief to improve overall fitness and activity levels. This involves (requires) retraining muscle memory from the myriad ways your body has developed physical coping mechanisms to minimize pain. I am 16 months out from surgery and still learning to avoid actions that had become second nature over previous decades. When I am out walking now, I frequently see walkers with the characteristic stiff hip and limp that comes from favoring a bad knee and joggers with the characteristic excessive knee hyperextension that signals a torn ACL.
Supplement:
At the suggestion of an undergraduate, the three authors of this article – Professor David M. Cutler, Professor Ellen Meara and Professor Susan T. Stewart took part in a two-week study into the practical effects of pain by taking up jobs in an Amazon Fulfillment Center. The three professors are expected to extend the information in this article just as soon as they are back from medical leave.
is this serious, or a sarcastic response?
good idea, nonetheless. but two weeks is not nearly enough. try 6 or more. and worry about paying the rent and utilities on top of it.
could be why lower income people are “depressed” thus experiencing more pain. also, the pressure of knowing you have to continue to do those kinds of jobs that increase your pain, or you will be homeless in short order.
i noticed they included no potential causes for “depression”. not that mine are correct, but they at least theorized some causes for “obesity”.
A few years ago a clerk limped badly as he guided me to the product I needed and winced as he turned toward me. I murmured sympathy and he said, yeah, I need knee surgery but I can’t afford it or the time off. How many of us in this country are in that position?
What get’s me are the pious fools and/or sadists in our culture who’d deny even cheap and safe pain medication to the poor if it causes the least bit of euphoria.
I’ve got news for them if they think they are doing God’s will; they ain’t – as they’d know if they read the Bible themselves (e.g. Proverbs 31:6-9).
Not long ago, my oncologist told me Tylenol with codeine is so dangerous, no one anywhere would prescribe it. Neither is true– you can buy it OTC in Canada and most countries except here. I only asked for Tylenol #3 as it is such a weak drug and I didnt want to argue over Percocet. Instead of prescribing, she denied I could be in pain and seemed miffed last time I saw her. I suppose I am now labeled a drug seeker.
Tylenol contains acetaminophen which can cause liver damage.
So apparently the sadists in charge consider dying of liver damage preferable to someone getting high off codeine.
… but even the compassion of the wicked is cruel. Proverbs 12:10
On the general point of pain management in the US (where I live), I would make the point that the general approach by the medical system is to do nothing until one has pretty severe pain, and then either (a) prescribe powerful drugs to mask the pain, (b) perform expensive and dubious surgical procedures to cut or remove the affected part, or (c ) prescribe “physical therapy”, i. e., a regimen of weird exercises further stressing the painful joint or area. Even if these things worked well, they all come too late.
A far better approach would be to eliminate the causes of chronic pain before they happen, but this is not considered part of the medical profession’s purview from what I can see.
” (c ) prescribe “physical therapy”, i. e., a regimen of weird exercises further stressing the painful joint or area.”
I agree that physical therapy can be uncomfortable, but sometimes the pain is necessary. I’ve gone to a physical therapist 3 times in my life. After a broken foot and sprained ankle, for severe shin splints, and for a messed up shoulder. I had been dealing with injury and pain for months (if not years in the case of shin splints). Each time I did exercises that were uncomfortable and seemed to make things worse at first, but over time, resolved the injuries.
The physical therapist said that one of the frustrating things about her job was that some people were unwilling to do any physical exercise or refused to do anything that was at all uncomfortable. Unfortunately, it often meant the problem just kept getting worse.
I’m not on the payroll for any physical therapist. I was initially very skeptical of it all, but it had a huge difference on my physical health. I would encourage people to give it a sincere effort. Of all my interactions with the medical system, the physical therapists have been of the most benefit.
A good PT can prescribe the right exercise that don’t stress the joint. A bad surgeon can remove/replace parts to cause more pain (and more money to his bank account). When it comes to choosing between surgery and physical therapy I’d pick the PT every time!
I was a little disappointed with this article mostly because Cutler and Stewart turned two topics I have great interest in – pain and socioeconomics – into a dry article. I frequently study pain in medical journals, but those don’t tend to discuss the financial and economic implications of pain. Whenever Yves writes about the intersection of human health and neoliberal finance, it’s utterly fascinating. But we already know she is quite skilled.
Studies that correlate physical impairments with educational status (or money) are important. More studies like this need to be done to illustrate the danger posed by the financialization of health care to the entirety of society.
Nevertheless, XXYY’s point about preventing the pain before it becomes chronically pathological is important. By the time a typical patient sees a doctor for musculoskeletal pain, that patient already missed multiple opportunities to prevent the escalation of pain. The doctor has ten minutes to decide on treatments or referrals, not nearly enough time. Worse, monetary pressures incentivize doctors to churn through patients and not focus on the fundamental trigger for joint pain.
In the case of knee pain, the article discusses BMI and outcomes for knee health, and it details how debilitating and disabling knee pain is. Unfortunately, it gives little practical advice on lowering the potential risk of knee injury. In utopia, your benevolent and unconstrained by time primary care physician would tell you about the danger of obesity, and you would, unconstrained by money, fix the obesity problem well before it causes the knee problem, amongst other things.
In my experience – I’m not a physical therapist or doctor, but I may pursue a PhD in the future – lifestyle changes and advice for properly loading knee and ankle joints are never given. I always check out the form of people walking and running, and a large percentage move in a way that, ceteris paribus, increases the chance of joint injury.
I spent a good amount of time studying the biomechanics of the human foot. Two major forces driving foot and knee injuries are shoes and excessive walking speed. These two are so common that nobody notices them. Nearly all shoes encourage the person wearing them to walk incorrectly and move excessively fast. This shodded gait transfers unnaturally high forces through the foot and to the knee. It might take years for these high forces to develop into pain. This process is, of course, accelerated by excessive body weight.
So here’s my practical advice. Slow down when you walk. And get rid of your shoes. Be very careful when walking barefoot because you need to unlearn some bad habits.
In my experience with arthritic knees, the PTs are the good guys, whose procedures and recommended exercises kept me from the doctors and surgery.
I will second that. My primary care doctor referred me to PT for arthritic knees about 9 years ago, when I was in my early sixties. I haven’t needed a doctor’s attention to knee pain since that time.
PAIN is why so many states have made medical marijuana legal. If you suffer from chronic pain, or have friends and/or family that do, you already know what opioid use and abuse look like or feels like. NO ONE wants to end up a junkie because of a bad back or knee.
Ultra conservative lawmakers like Nebraska’s receive plenty of Big Pharma money to keep medical marijuana criminalized… but voters and taxpayers SEE THIS and are unwilling to roll over and die when safer pain relief is readily available.
https://my.vanderbilt.edu/marijuanalaw/2019/08/nebraska-attorney-general-gives-the-state-some-bad-legal-advice-concerning-marijuana-legalization/
For me, my worst-in-a-lifetime chronic pain was 100% psychological. Once I recognized that fact, I got rid of the pain. I’ve told my story here before, and I’m stickin’ to it.
Two book recommendations:
1. Unlearn Your Pain by Howard Schubiner, MD. Link: https://www.unlearnyourpain.com/
2. Healing Back Pain by John Sarno, MD.
I read Dr. John Sarno’s book based on your prior recommendations. It’s excellent! Thanks!
Glad I could help!
+ 1 re. Sarno!
I don’t ‘ know if knee pain or political pain (pain in the neck) is the more acute. I suspect fixing political pain would work wonders for many, if not most, conditions.
pain is difficult to quantify…there’s no meter they can plug into you to measure your pain level….let alone distinguish “real” physical pain from the psychologically modified kind(yes, the latter is real…but it seems it’s too often an excuse to dismiss/ridicule). all we’ve got is the little chart of smiling=>frowning faces. this requires a modicum of trust of what the patient says.
i’ve been painful for 30+ years…and one does learn to live with it, and to go through it…at least up to a point.
the injuries that cause the pain in the first place are sometimes not overcomeable.
i finally got a hip in 2013, after being laid low for almost 7 years waiting for our deplorable public health system to kick in.
I’ll likely not be able to get an ankle unless $$$ falls from the sky and i can make a run to Cuba.
my knees and my back, similarly, are likely beyond any hope of relief.
but i soldier on…because what else can i do?
i like to call it Bruxist Tenacity…it’s the grit teeth that holds up my carcass.
i’ve taken hydrocodone for 16 years, with periodic, self imposed “drug holidays”(had to educate my doctor about this)…both to “reset the receptors” prolonging the efficacy of this drug, as well as making sure i’m merely “dependent”, rather than addicted (zero withdrawal symptoms, ever…just the pain)
i also smoke a lot of pot.
and, after the hip replacement, and habitually laying around for hal;f a year, because i couldn’t figure out what to do with myself…i started building things out here on the farm.
like this house. art project/physical therapy.
nobody wants to believe you if you say youre in pain…and no one wants to run up the pain ladder to opiates, because of the opioid deaths of despair and addiction. i was shocked, to say the least, to discover this phenomenon…the assumption that i was lying,lol.
trying to get high…or “on welfare”…its degrading and insulting.
it took me years to get my regular doctor to finally let me try vicodin…and i had to beg to be kept out of a “pain management clinic”(my pot use is a giant red flag for those people, to this day)
a big part of my current condition is the effect of having to not get treatment, back when it would have been relatively simple to do so, if i had only had “access” to the “greatest healthcare in the history of the world”(tm)
but i didn’t, and i worked like the dickens for all that time, instead…restaurants, mostly.
lack of such access is the number one reason i’m in the shape i’m in, today…not hard living(although that contributes) or loose morals, or whatever other excuse they invent.
i had to simply endure broken and otherwise damaged bones and joints…because i’m not worthy.
i’m not in the club.
pain…specifically arthritis…has been #1 in this country for a long time.
it’s obvious, to me, why that is.
we’re cattle…beasts of burden.
…mustn’t grumble.
Well said. I trashed a knee in my stupid youth in 1979. Despite having more or less decent insurance through the years, I spent the first 30+ years afterward on a cycle of ignoring it and then, periodically, being laid up through further use, until I felt good enough to ignore it again. (I finally had it scoped in 2001, which only made the pain worse.) As you say, pot makes a huge difference – though I never shared this finding with anyone in health care. And stretching, for which the pot is also a good motivator. Thankfully, I haven’t had to work a standing job since I was a young man. I couldn’t have. (Restaurant work – I call that hard living.) But even so, aging and arthritis take their toll and after a number of years of very constricted activity, I was finally persuaded to get a new knee last year. Glad I did.
You hit Medicare-eligible any time soon? As I noted above, at least in this part of the world, Medicare seems to be willing to pay for joint replacement with few questions asked. Not sure about ankles though.
i’m 51.(people who see my xrays, etc say they look like xrays from an 80 year old)
medicare is either 62 or 65(i can never remember).
and i am loathe to attempt medicaid/ssi in texas again…all the bullshit and threats and the default assumption of fraud…as well as asset limits(beat up trailer house, whatever else is in dad’s will) and skating along the upper limit of the income cutoff. i doubt that i’m even eligible.
…which is ludicrous, in and of itself.
I know my limits, as far as tasks i just shouldn’t even attempt…once all this infrastructure frenzy is done, i can sink back into my farmer groove.
(the purpose of well planned infrastructure is saving labour later, and enabling that Farmer Groove in the first place)
That’s what struck me as so crazy about my fellow new knee people: on most I have to think the effort is more or less wasted whereas there are so many people whose lives would be dramatically improved but aren’t allowed. Absurd. And cruel. And thus completely normal.
aye! all those years that i was hacking my way through the Disability Maze, i knew many local ancients(80-90) who would take extended tours around town to show off their new hip/knee/shoulder.
i reckon this is part of the reason for the widespread disbelief from said olds(including my dad and stepmom) regarding my insane difficulty with healthcare….they never had a problem getting the care they needed(or even just wanted).
hell…stepmom…she of the bad back…(and beneficiary of dad’s largess) had no difficulty at all getting Disability…or vicodin, either(profiling).
i try to control for my hypercynical nature,lol…but it’s almost as if it’s all designed to not help those who need it most.
i was 37(i think) when i had to “retire”. I’d likely still be poor if i had been able to keep working, but still…
I’ve had my eye on this book, might be of interest to some here
As someone who’s had severe knee and leg pain for years, that limited my ability to walk and stand, limited the range of motion of my legs so I could not bend them very far even with high pain, I can confirm complete resolution in about a month with only one change. Change in diet. Fat free, plant based, no animal sources or alcohol. That’s all. When I tried to reintroduce any of them, it came back. I’m nearly 70. Your mileage may vary. Total cost: reduced grocery bill. Availability: universal