Yves here. KLG warns that this post wound up not quite where he expected, which suggests he had to refine/revise his impressions based on investigation and reflection.
A big issue is humans are already variable enough even before getting to issues of habit and diet that even well-conducted research is fuzzy save perhaps for very particular interventions that can be expected to have an impact (or not) quickly, plus with little reason to expect long-tail impacts.
KLG raises an additional issue, in that practitioners are under pressure to deal with immediate needs (what MBA love to call decision making under uncertainty) while scientists have the luxury (if they have the budget!) of building big samples and if their research was well designed, having high to very high confidence in their findings.
By KLG, who has held research and academic positions in three US medical schools since 1995 and is currently Professor of Biochemistry and Associate Dean. He has performed and directed research on protein structure, function, and evolution; cell adhesion and motility; the mechanism of viral fusion proteins; and assembly of the vertebrate heart. He has served on national review panels of both public and private funding agencies, and his research and that of his students has been funded by the American Heart Association, American Cancer Society, and National Institutes of Health.
There has always been something to complain about when considering the practice of biomedical science, and we have highlighted some of these here over the past two years. For example, Evidence-Based Medicine (EBM) sounds very promising on the surface. The term is often used uncritically as something inherently good. EBM is the accepted and expected practice taught in medical education. But EBM can also consist of special pleading from Big Pharma, when the descriptive term “Biomedicine” should be applied [1].
Still, biomedical scientists often get it right, and this must also be appreciated. To deny this would be churlish if not downright obtuse, but churlish and obtuse describes our political talk these days. Most significant biomedical discoveries are made with public support, including that from nonprofit organizations such as the Hereditary Disease Foundation. Big Pharma also had an essential role into the late-twentieth century in basic biomedical research(Gertrude Elion and George Hitchings at Wellcome Research Laboratories in Research Triangle Park, NC). Big Pharma has always been essential for optimization, production, and distribution of novel drugs. Alexander Fleming discovered penicillin at London University in 1928 and it was synthesized by Howard Florey and Ernst Boris Chain at Oxford during World War II [2], but its breathtaking utility in saving lives, initially near the end of WWII, depended on production and distribution by what has come to be known as Big Pharma (with major support of the United States and British Governments). The latter is also true of vaccines that have saved countless people from death or debility from preventable diseases: MMR, DTAP, cholera, smallpox, measles, and HPV. The list is long.
Cancer is and will remain a scourge for the foreseeable future, but modern clinical oncology works wonders in certain cases. I had a recent personal experience that would have been much more difficult twenty years ago than it was in 2022 because clinical oncologists and basic biomedical scientists have been hard at work improving their strategy and technique. Instead of surgery first, which would have been debilitating, followed by relatively unfocused radiation and untargeted chemotherapy, my treatment consisted of powerful, focused and tunable radiation along with an optimized course of chemotherapy that avoided the ancillary damage to my mouth, throat, kidneys, and eyes, which was often associated with earlier treatment. The final PET-CT scan result was “Hypermetabolic signal (cancer) completely resolved; no further treatment (e.g., surgery) recommended at this time.” Fingers remained crossed over a thankful heart.
I have been an apprentice or working biomedical scientist since the late-1970s. Advances have been remarkable, but the problems we face as a scientific community and polity remain more difficult than they should be. The ups and downs and ebbs and flows of biomedical research are well illustrated in our long history with diabetes. This is covered in his usual exceptional detail by Gary Taubes in Rethinking Diabetes: What Science Reveals About Diet, Insulin, and Successful Treatments (2024). Gary Taubes is a reporter, not a scientist. Full disclosure: I have read each of his books and find him to be authoritative despite my occasional puzzlement or his misuse of a scientific term that would be noticed only by the biochemist or cell biologist [3]. I view him as the equivalent of David Halberstam and Neil Sheehan (War in Vietnam), Brian Deer (Andrew Wakefield and his totally spurious connection of MMR to autism that granted the gift of eternal life to vaccine denialism), John Carreyrou (Elizabeth Holmes and Theranos), and Horace Freeland Judson (modern molecular biology).
Each of these writers is an authoritative reporter/historian/analyst from which the interested reader will learn about something important. The scientist, too. No modern molecular cell biologist can be a good scientist without understanding everything in Judson’s The Eighth Day of Creation: The Makers of a Revolution in Biology. A few graduate students I have taught have listened to me and agree, and a few medical students have also listened and learned much from Siddhartha Mukherjee’s The Emperor of All Maladies: A Biography of Cancer. But too few. Any scientist connected to medicine or medical education who is willing to read will also learn much from Taubes.
The fundamental difficulty, or incongruency, between biomedical science and scientific medical practice can be summed up as follows:
The goal of biomedical science is to establish reliable knowledge that guides medical practice. This dovetails with Nancy Cartwright’s view that scientific knowledge must be reliable rather than the “truth,” although reliable knowledge will contain much provisional truth. Scientists have the luxury of time to get it right while working meticulously through ambiguities and challenges, provided the necessary support is available.
On the other hand, physicians do not have this luxury: “Their patients are sick, and treatment cannot be postponed for the years or decades required for clinical trial results that might tell then the best course of treatment – if, indeed, such trials are even planned or underway.” (emphasis in original)
This tension has permeated diabetology for well over 100 years. The first modern discovery in diabetes probably dates to 1889, when Oskar Minkowski surgically removed the pancreas of a dog. The goal of his research was to determine the function of the pancreas, which was known to be a secretory organ. The result was that the dog, who was house-trained, suffered from polyuria (excessive, involuntary urination) and polydipsia (excessive drinking). As the good chemist and scientist he was, Minkowski tasted the urine. It was sweet [4].
The natural and correct, but not complete, conclusion of this experiment is that loss of the pancreas leads to loss of control of carbohydrate (sugar) metabolism. This observation has colored every aspect of diabetology since. The late J. Dennis McGarry published an article in 1992 in Science entitled What if Minkowski had been ageusic?, i.e., lacking a sense of taste (alas, behind a paywall). He would not have noticed the glucose, but he might have noticed the smell of acetone (the active ingredient of nail polish remover). This would have implied that fatty acid metabolism [5] was also dysregulated in diabetes, something well understood now, but often as an afterthought, even as scientists are still “grappling with the enormous complexity of a disease process in which almost every aspect of the body’s metabolism goes awry.” The lesson from McGarry is:
The order in which scientists learn something is likely to determine how they think about it, right or wrong, ever after. Since Minkowski, diabetes had been a disease of sugar metabolism and not due to the global dysregulation of metabolism.
This has led to the cognitive dissonance in diabetes research, which is refracted by the different imperatives of scientific medicine and biomedical science: Do something now for the patient versus determine what is useful and true, however long this takes and then do something for the patient if you can. Early clinical interventions placed patients on high-fat diets with lower levels of carbohydrate and protein and their condition improved, often remarkably. But the paradigm was set: Diabetes (both types) is a disease of sugar metabolism. When insulin was shown to “cure” Type 1 diabetes 100 years ago, the focus became locked on insulin and the maintenance of low-glucose urine (and blood, but that was more difficult to measure at the time). Fat and cholesterol were later demonized incorrectly as the cause of heart disease.
This led to the replacement of fat calories with refined carbohydrates. This has been a subject of Taubes and others and has been reviewed previously here and here. The fairly obvious result has been the obesity epidemic in countries afflicted with the so-called Western Diet. The reasonable conclusion is that the high-carbohydrate diet leads to high insulin levels. Insulin is our primary anabolic hormone. When we are in the fed state, it tells the body to make fat in the liver and store fat in adipocytes (fat cells). Too much insulin and fat is stored at adventitious sites such as the liver (fatty liver disease). Diabetics were later advised they could eat whatever they wanted, within reason, and let insulin cover the excess carbohydrates. This resulted in poor glycemic (glucose) control and later complications. More recently, it has been shown that consumption of, not eating, ultra-processed foods leads to increased consumption of carbohydrate-laden food-like substances and then to more obesity. But it seems clear to me the sugar came first. UPF are loaded with sugar.
So where should diabetologists and our decrepit healthcare system go next? This is where Taubes will likely raise the sharpest hackles among the scientific community. It is unquestionable that insulin has been the lifesaver it was 102 years ago when Billy Leroy was an early patient to be treated with insulin. He was three years old and weighed 15 pounds after suffering with diabetes for two years. After three months on insulin his body weight had doubled and he was an attractive, robust little boy who could handle a shovelful of snow (Figure 7 from Robert Tattersall, Diabetes: The Biography, p. 62; Oxford University Press, 2009).
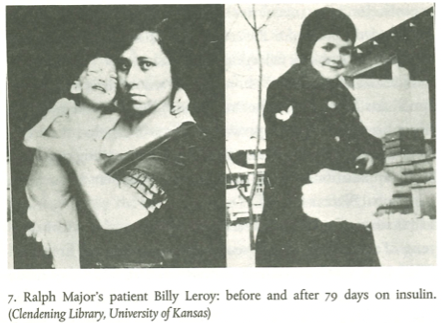
The awe in which insulin is rightfully held, and the before/after photographs of Billy Leroy are awesome in every sense of the word, is also related to the fact that when insulin was introduced the only available drugs that worked as advertised were, for the most part, morphine, aspirin, phenobarbital, and digitalis. Insulin treated the apparent primary symptom of diabetes very well – high blood sugar – but did little in and of itself to prevent sequelae of the disease. Instead, a series of ad hoc but extremely useful treatments have been developed for those: Blood pressure medicines for the high blood pressure associated with diabetes, laser surgery for retinal hemorrhages caused by insulin- and glucose-mediated damage to the microvasculature, advanced wound care for diabetic lesions caused by poor circulation in the legs and feet that often result in amputation, dialysis machines for diabetic kidney disease, statins for diabetic coronary heart disease, new and improved insulins that go back to the 1930s when additives were used to increase the half-life of insulin in the circulation, insulin pumps that work better and more unobtrusively [6]. These interventions work, and patients with Type 1 diabetes typically do well. But not all patients.
Recent clinical observations have shown that low-carbohydrate, ketogenic diets manage carbohydrate load well and keep the patient healthy and euglycemic (normal glucose concentrations). It is clear that patients with Type 2 diabetes (insulin-resistant diabetes) can do well on low-carbohydrate diets. This is also true with some Type 1 diabetics, who have had success controlling their systemic glucose levels with diet. Insulin may still be necessary in most of these patients but at much lower therapeutic levels than usual. And this is the proper direction for the future. A significant number of diabetologists have always considered that daily, high-dose administration of insulin is probably not healthy in the long run. They are correct. Moreover, in a non-diabetic patient with a properly functioning pancreas, less than 50 percent of secreted insulin escapes the liver. It is extremely likely that so-called off-target effects in diabetics such as arterial stiffness are caused by the subcutaneous injection of insulin that results in high systemic insulin load compared to endogenous insulin.
Which brings us to the next level. The culture of “Yes, we have a pill (or shot) for that!” has ultimately given us Glp-1 (glucagon-like peptide 1) receptor agonists (Wikipedia link but the explanations are correct if simple). These drugs were developed to treat Type 2 diabetes. The following summary of the proximal physiology is well understood, while the interpretation is loaded with wishful words:
Glucagon-like peptide-1 receptor agonists (GLP1RA) augment glucose-dependent insulin release and reduce glucagon secretion and gastric emptying, enabling their successful development for the treatment of type 2 diabetes (T2D). These agents also inhibit food intake and reduce body weight, fostering investigation of GLP1RA for the treatment of obesity.
The actions of GLP-1 to reduce food intake and body weight are highly conserved in obese animals and humans, in both adolescents and adults. The well-defined mechanisms of GLP-1 action through a single G protein-coupled receptor, together with the extensive safety database of GLP1RA in people with T2D, provide reassurance surrounding the long-term use of these agents in people with obesity and multiple co-morbidities. GLP1RA may also be effective in conditions associated with obesity, such as cardiovascular disease and non-alcoholic steatohepatitis (NASH). Progressive improvements in the efficacy of GLP1RA suggest that GLP-1-based therapies may soon rival bariatric surgery as viable options for the treatment of obesity and its complications.
The long-term effects of treatment with these peptide hormones are unknown and cannot be assumed to be benign. In my view this places the use of these drugs to treat obesity firmly in the fundamental scientistic category of “technical solution for a problem that shouldn’t exist.” The use of Ozempic for cosmetic weight loss may also lead to “Ozempic Butt” (a relatively safe click if you must) or Ozempic Face caused by the concomitant loss of lean muscle mass. I experienced lean muscle loss as a side effect of my cancer treatment. It is miserable and not easily reversed.
A healthy diet, for most people, would solve these problems. A healthy food culture that leads to healthy people can be regained. We had one not so long ago. Yes, this can be done. The problem is one of political economy, not pharmacology and not biomedical science or scientific medicine. There are no laws of political economy that prevent this recovery because there are no laws of political economy, only conventional wisdom. Which is not. When we develop the will, the routes will be as varied as geography. In the meantime, I highly recommend Rethinking Diabetesas a guide to thinking about how biomedical science and scientific medicine are similar and different, especially if detail appeals to you. A strong rational and observational, if somewhat hidden, scientific foundation supports Taubes’s presentation. Heterodox clinicians whose concerns lie with the patient holistically rather than as a congeries of symptoms of the condition to be treated using the products of Biomedicine, will lead the way. EBM, properly focused, will follow scientific medicine and biomedical science, as it always should.
Finally, this would also go a long way toward restoring trust in the medical establishment that has been eroding for 40 years, most of my working life, and catastrophically in the last four years. During this time the leaders of Biomedicine chose not to remember what they (should) have known for more than 50 years, unlike the original diabetologists who were acting intelligently but often in a semi-blind state: Lasting immunity to coronaviruses, whether by vaccination or previous infection, is a unicorn. Thus, we have mRNA vaccines that are as novel today as insulin was 100 years ago. Also revolutionary. Also very profitable. The imperative of Biomedicine this time was to “Do something now!” Understood. But the scientific foundation had already established that this something was unlikely to work. And it has not worked by the standards the people have come to expect of vaccines. COVID-19 vaccines prevent neither the disease nor its transmission. They might lessen the serious of the disease, but much of that can be attributed to better, learned clinical management. Alternative approaches analogous to the modified diet that relieves diabetes have languished, so far. Millions have died. The only solution to this is to reconcile the biomedical science of COVID-19 with the scientific medicine of clinical practice. This can be done, too.
Notes
[1] This would include much of the output of Big Pharma, which has become primarily the marketing arm of the giant legacy pharmaceutical companies that were established in the nineteenth century and their more recent competitors. The notion that Big Pharma needs big sales to support big research is simply not true despite their protestations to the contrary.
[2] My first mentor in biochemistry (98 years old in 2024) was a Corpsman (Medic) in the US Navy during the latter stages of WWII. He told the story of giving an injection of penicillin to a sailor who would have perished from bacterial pneumonia by the following morning. Instead, the patient was wide awake and hungry when my older friend returned to duty the next day, something that had never been seen before in his experience.
[3] For example: The LDL particle is not a molecule; it is a particle comprising thousands of different molecules – lipids, proteins, and cholesterol. Cholesterol is not a fat. But cholesterol and fat have been conflated in the common lay, and medical, understanding of metabolic disorders with a dietary etiology. It turns out that cholesterol is not the “molecule of concern” that this common understanding still maintains. In Rethinking Diabetes Type 1 and Type 2 diabetes are sometimes not distinguished explicitly from one another, but the general point of the book is that this may not be entirely necessary when taking a holistic view of metabolism dysregulated by too little (Type 1) or too much (Type 2) insulin that cells ignore.
[4] The dog was urinating uncontrollably because glucose spilled over into his urine and as a very hydrophilic (water loving) molecule the glucose carried additional water with it. This water loss was corrected by excessive drinking. These are two signal symptoms of the onset of Type 1 diabetes (previously called juvenile diabetes) in humans. Type 1 diabetes is caused by destruction of insulin-producing cells of the pancreas. Without insulin the liver and other organs do not take up glucose from the circulation, leaving the blood and urine with excessive glucose. This circulating glucose causes much of the damage in diabetes because it reacts non-enzymatically (irreversibly, called glycation instead of glycosylation) and tags and crosslinks normal cellular proteins, rendering them permanently nonfunctional.
[5] (TMI) Acetone is a 2-carbon compound and fatty acids are metabolized in 2-carbon units, with acetone a terminal product of fatty acid oxidation. Carbohydrates are metabolized as 6- and 3-carbon units. The 2-carbon units of fatty acids cannot be used to synthesize carbohydrates but carbohydrates will be converted into fatty acids under the influence of insulin, our primary anabolic – i.e., building – hormone. This is why patients with Type 2 diabetes are often obese. Type 2 causality goes in both directions: obesity leads to insulin insensitivity which leads to Type 2 diabetes which leads to more insulin insensitivity…
[6] Despite statin over-prescription for the past 30+ years coronary heart disease (CHD) is still the leading cause of death, maintaining its lead over cancer. One would think that if statins are the lifesavers advertised, these numbers would change, but I digress. Which is not to say that statins are not useful in people with serious disorders of cholesterol clearance or diagnosed CHD. Or that statins reduce chronic inflammation, which is a recent excuse for their continued general use. This may be true, but losing weight also reduces chronic inflammation.


‘A healthy diet, for most people, would solve these problems. A healthy food culture that leads to healthy people can be regained. We had one not so long ago.’
I agree with the sentiment but I am no longer confident that today’s medical establishment is capable of giving solid guidelines on what a healthy diet consists of. Not after the Covid response fiasco. So will guidelines come out telling people to try to eliminate as much sugar as possible from their diet and having the government put a tax on any drink or food containing sugar? The sugar industry would never stand for it and would fight it behind the scenes with a ruthlessness that would make AIPAC blush. Any movement for a real healthy diet will not come from the top down but will have to start at the base.
I agree with your conclusion, but if I were dreaming about a better top down response, it wouldn’t be for the government to step in with social “nudges.” Why not dream big.. the major food players could stop pretending “low fat” is healthy, and stop all the added sugars. They could switch from seed oils to healthy animal fats. I guess they could have their lobbyists rewrite the guidelines too while they’re at it, lol.
And yet there seems to be no answer to the life threatening disease of poverty, especially in the “first” world, which should be an easy fix since “money” is created out of whole cloth. One is either too poor to afford a good diet or will be poor soon enough should one require the advanced medical treatments that have lead to an epidemic of medical bankruptcy. And it seems to be getting worse – see the dismantling of the UK’s NHS or the “death by spreadsheet” economics of the US health insurance model.
Brilliant!
Thank you for this well-written and perceptive article. I, too, am a fan of Taubes. One of the advantages of living a longer life is being able to reflect on general health conditions over the years. As a kid, in a rural public school, I remember maybe one 12 year old out of twenty being fat. Sixty years later, we’re in the 4-6/20 range, depending on how you define obesity. The primary reason is no mystery: 85% (picking a number out of the air!) of the stuff sold at your average supermarket is bad for humans. . . at any quantity. Yes, sadly, there are genetic dispositions for some; but the primary, ongoing, life-threatening epidemic in my lifetime is diet-caused obesity (with a small nod to increasingly sedentary lifestyles).
As KLG hints at, the good news is that families and individuals can do something about this. The bad news is that the forces arrayed against trying to lead a healthy life–food and beverage companies, supermarkets and restaurants, misguided government institutions, and the media–are hyperpowerful and omnipresent.
Forgot to add a note about how buying decent food at a supermarket is just a start. One has to know how to prepare it into an appetizing meal, and have the time to do so. Well, that’s a key issue in stressful times. Perhaps a silver lining to the peak covid period was the reevaluation by many of the basic rhythm of life. Overconsumption and overconvenience are the enemies of good health.
I’m reminded of Michael Pollan’s advice for a healthy life:
Eat food.
Mostly plants.
Not too much.
And when he says “food” he doesn’t mean industrially processed food-like substances.
I feel like it will all be knitted together soon. Or eventually. The COVID spike protein is interesting. Maybe one of several keys. Locks and keys. It is via the ACE receptor that COVID’s spike protein enters the human cell. I take a BP pill that is an “ARB” which blocks the ace receptor (if I understand this, it is the same receptor that connects with COVID’s spike protein) and I learned by reading up that my BP med (losartan) reduces the intensity of a COVID infection because it blocks the same receptor. It doesn’t prevent infection. I’ve had COVID twice. But not too seriously and never in my lungs; always intestinal. So I recently went out to read up on losartan again and found yet another benefit – losartan also helps prevent tumor formation. I can’t remember if this is also connected to the ace receptor or another ubiquitous little spike protein. But it seemed like reasonably good news. Maybe it could be a maintenance drug. Or could lead to one.