Readers, I’m sorry this is a bit late. The “T” on my keyboard gave out, and with an already dodgy “N” it was simply too much. I had to switch to a second machine, and that wasn’t as seamless a transition as I might have wished. –lambert
By Lambert Strether of Corrente.
I encountered a new KHN article with the eye-catching title “Avoidable Sepsis Infections Send Thousands Of Seniors To Gruesome Deaths,” but discovered it was both what, and less than, it seemed. The article was quite strong on sepsis[1] horror stories in nursing homes, but less strong on epidemiological data. So I’ll present extracts from KHN, and then broaden the scope of the article to sepsis generally, for which we have a wealth of information. (Kaiser also has this handy interactive map, “Pinpointing Sepsis Risk, By Site,” that allows you to search for nursing homes — although not hospitals — by state and city, in case the combination of my headline and KHN’s headline has given you apprehension. All nursing homes aren’t death traps, fortunately.)
First, the KHN article. Skipping the horror stories, the numbers:
Year after year, nursing homes around the country have failed to prevent bedsores and other infections that can lead to sepsis, an investigation by Kaiser Health News and the Chicago Tribune has found….
A special analysis conducted for KHN by Definitive Healthcare, a private health care data firm, also suggests that the toll — human and financial — from such cases is huge.
Examining data related to nursing home residents who were transferred to hospitals and later died, the firm found that 25,000 a year suffered from sepsis, among other conditions. Their treatment costs Medicare more than $2 billion annually, according to Medicare billings from 2012 through 2016 analyzed by Definitive Healthcare.
In Illinois, about 6,000 nursing home residents a year who were hospitalized had sepsis, and 1 in 5 didn’t survive, according to Definitive’s analysis.
Understaffing is one possible cause of sepsis:
Much of the blame, regulators and patient advocates say, lies in poor staffing levels…. Matt Hartman, executive director of the Illinois Health Care Association, which represents more than 500 nursing homes, acknowledged low staffing is a problem that diminishes the quality of nursing care.
Hartman blamed the state’s Medicaid payment rates for nursing homes — about $151 a day per patient on average — which he said is lower than most other states. Medicaid makes up about 70 percent of the revenue at many homes, he said.
(The article says nothing about staffing at profit vs. non-profit facilities). Nevertheless:
There is little agreement over how much staff should be required in nursing homes. Federal regulations simply mandate that a registered nurse must be on duty eight hours per day, every day. In 2001, a federal government study recommended a daily minimum of 4.1 hours of total nursing time per resident, which includes registered nurses, licensed practical nurses and certified nursing assistants, often referred to as aides. That never became an industry standard or federal regulation, however.
Most states set requirements lower and face industry resistance to raising the bar. A California law requiring 3.5 hours per resident as of this July 1 is drawing intense criticism from the industry, for instance.
A second cause of sepsis, no doubt related to staffing, is poor infection control:
Poor infection control ranks among the most common citations in nursing homes. Since 2015, inspectors have cited 72 percent of homes nationally for not having or following an infection-control program. In Illinois, that figure stands at 88 percent of homes.
Finally, sepsis often leads to hospitalization, stressful for patients and expensive:
[A] federal report has found that care related to sepsis was the most common reason given for transfers of nursing home residents to hospitals and noted that such cases ended in death “much more often” than hospitalizations for other conditions.
Examining data related to nursing home residents who were transferred to hospitals and later died, the firm found that 25,000 a year suffered from sepsis, among other conditions. Their treatment costs Medicare more than $2 billion annually, according to Medicare billings from 2012 through 2016 analyzed by Definitive Healthcare.
“This is an enormous public health problem for the United States,” said Dr. Steven Simpson, a professor of medicine at the University of Kansas and a sepsis expert. “People don’t go to a nursing home so they can get sepsis and die. That is what is happening a lot.”
Nevertheless:
No one tracks sepsis cases closely enough to know how many times these infections turn fatal.
That’s what I mean about there not being enough epidemiology! A second example, on hospital transfers:
[A] critical 2013 Department of Health and Human Services audit found Medicare had paid about $14 billion in 2011 for these transfers. Care related to sepsis cost Medicare more than the next three costliest conditions combined, according to the audit.
The auditors have not checked in to see if Medicare has since reduced those costs and have no plans to do so, a spokesman for the HHS Office of Inspector General said.
Now let’s turn to sepsis at the national level, for which there is a wealth of information. First, some numbers. Sepsis is a terrible problem:
Sepsis is associated with a high mortality rate and poses an overwhelming burden of healthcare utilization in the United States. In the United States sepsis is a major public health problem responsible for over 750,000 hospitalizations and 215,000 deaths annually.
It’s not clear how many of those hospitalizations are transfers from nursing homes, since we have no data. It’s also not clear to me how much sepsis is caused within — or by — hospitals; clearly a lot, since “there were an estimated 722,000 [Hospital Acquired Infections (HAIs) in U.S. acute care hospitals” in 2011; however, not all HAIs culminate in sepsis. From the NIH:
Sepsis is a major challenge in hospitals, where it’s one of the leading causes of death. It is also a main reason why people are readmitted to the hospital.
What is clear is that people who, for whatever reason, are more likely to have become enmeshed in the health care system are also at greater risk. From the NIH once more:
The people at highest risk are infants, children, the elderly, and people who have serious injuries or medical problems such as diabetes, AIDS, cancer, or liver disease.
As we might expect, sepsis is not uniformly distributed. Two factors seem salient: Household income, and geography.
First, household income. From “Association of Household Income Level and In-Hospital Mortality in Patients With Sepsis: A Nationwide Retrospective Cohort Analysis” (2018):
Associations between low socioeconomic status (SES) and poor health outcomes have been demonstrated in a variety of conditions. However, the relationship in patients with sepsis is not well described. We investigated the association of lower household income with in-hospital mortality in patients with sepsis across the United States.
After adjustment for severity of illness, patients with sepsis who live in the lowest median income quartile had a higher risk of mortality compared to residents of the highest income quartile. The association between SES and mortality in sepsis warrants further investigation with more comprehensive measures of SES.
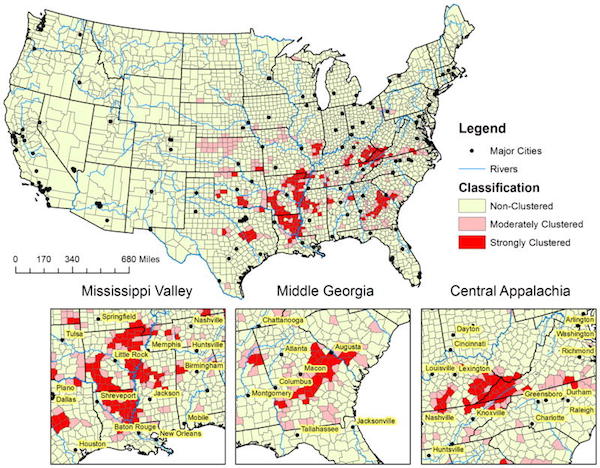
Second, geography. From “Defining Sepsis Mortality Clusters in the United States” (2017):
These results also suggest that sepsis mortality clustering is prevalent in counties located in the southeastern US with three specific clusters: 1) “Mississippi Valley” – counties bordering the southern Mississippi river in three southern states (Louisianna, Arkansas, and Mississippi); 2) “Middle Georgia” – a belt of counties expanding from southwest Georgia through middle to southeast Georgia; 3) and “Central Appalachia” – a cluster of counties in southeastern Kentucky and southwest Virginia…. Over the ten-year observation period, 5.2% (161 of 3,108) of US counties were defined as strongly clustered counties. After adjustment for age and community level characteristics, those living in the strongly clustered counties were about 1.5 times more likely to have a sepsis related death than people living in non-clustering counties. Demographic and socio-economic characteristics associated with sepsis mortality clustering were race, household income, value of housing property, education, rural population, poverty, ratio of hospitals per 100,000 persons, insurance coverage, and higher unemployment rate.
Here’s a map of the authors’ county level data:
(They prescribe ACA expansion, because most of the mortality clusters are in non-Medicaid states, but if the objects is to impose uniform standards of care, surely Medicare for All would be better?
As usual in our wonderful health care system, some go to Happyville, and some to Pain City, depending on the luck of the draw. If you want to avoid sepsis for yourself or a loved one, clearly your best approach is to pick wealthy place to be born, and plan to avoid growing old; failing the latter, you can to some extent be a “smart shopper,” at least for a nursing home, by using this interactive map. While I was doing the research for this piece, I ran across a lot of work by practitioners seeking to prevent sepsis — the slide in note [1] is from a conference on the topic — and that makes me hopeful, but when that good work comes to fruition, it will surely do so based on income and geography, and the unfairness of that — particularly for the helpless elderly — makes me heartsick.
NOTES
[1] What is sepsis? In medicalese: “Sepsis should be defined as life-threatening organ dysfunction caused by a dysregulated host response to infection” (The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3)). In lay terms: “Sepsis is the body’s overwhelming and life-threatening response to infection that can lead to tissue damage, organ failure, and death. In other words, it’s your body’s over active and toxic response to an infection” (Sepsis.org). Here is a tweet on how to detect sepsis in its early stages:
Pippa Bagnall Sepsis can happen to anyone anytime. Community Nurses can be 1st to identify; know the symptoms #qni2018 pic.twitter.com/8YrkRir32Z
— Anne Taylor RGN DN QN MSc (@AFTaylorDN) September 24, 2018
Note especially that next-to-the-list bullet point. The initials of each bullet point spell “SEPSIS”; this is “I.” Yikes.


Chilling.
My mother developed sepsis about two weeks after a stent was put in. There was no clear evidence that was the cause but it is considered the most likely. Fortunately, we were home at the time things went down hill. Had we been at work, she would have likely died.
In case it helps someone else…
She said she wasn’t feeling well and wanted to lie down. Within an hour, she developed acute diarrhea like nothing I have ever seen before. I called the 24 hour nursing hotline for her healthcare provider. While on the phone, the nurse said, “if she starts throwing up what looks like coffee grounds, call an ambulance.” The words were no sooner out of her mouth, when it started. I hung up, dialed 911 and an ambulance was at our house in about 10 minutes (we live close to the dispatch center)
At the hopsital, the ER physician said there wasn’t time to find out what caused it, what was clear was she had a massive infection and they needed to aggressively start treatment.
Later that night she was transferred to a cardiac care unit where she spent the next four days. Once she stabilized, she was transferred to a nursing facility for another 10 days of intravenous antibiotics. While in the nursing facility, she acquired Clostridium difficile (c-diff) which was easily cleared while she was home.
Why tell this story? We had several key advantages that contributed to a successful outcome.
My mother lives with us so she has accessible care givers around her
We were home at the time
Her health care provider has a 24 hour nurse practitioner help line
911 is in operation in our area
Ambulance services are close to us
The hospital is close to us
The nursing facility she was sent to has a good record
If you take one of those away, I am fairly certain she would have become another sepsis mortality figure.
As I said somewhere else on this thread, disposable income is the gateway keeper. We would have a hard time finding a 24hour anything around here that took Medicare. I’m glad your Mom made it. I’ve had stents put in, and it’s no fun.
Your mother’s case is one of what is called nocosomial sepsis or nocosomial disease, or sepsis related with invasive health care. My guess is that, in many cases sepsis in nursing homes will be related with such operations (injections, probes, stents…). The elderly are at highest risk for these diseases together with inmunodepressed. Also, due to higher antimicrobial consumptiom in nursing homes, resistant microbes are also common. A typical one and probably the most prevalent among the elder is meticillin resistant Staphylococcus aureus followed by multiresistant E. coli strains.
Another difficulty is that simptomatology among the elder is quite different from the rest of the population and it is more difficult to stablish good treatment protocols. Thus treatmets are tipically “empirical”. In Spain highest rates of sepsis among the elder are prevalent in short stay centers visited for health care.
It surprises me that there is not good tracking of sepsis in the US.
As you say good practices is the bestr way to avoid these sepsis cases
It appears that in our country, they didn’t have a hard time figuring out how much money was “spent” on septic patients. Clearly, that took priority over people. Sadly the types of sepsis and predisposing diagnosis etc isn’t followed nationally. Some people who acquire nosocomial infections have predisposing conditions that make their health compromised going into a facility. But frequently, inadequate staffing, staff that may not follow protocol or cut corners, language barriers, loss of interest in the job, etc., inadequate infection protocol/procedures are the reason that these infections rise to the top. Antibiotic resistant infections have been charging forward for the last decade. We were warned. We ignored, and now, we all pay the price
Greetings ‘O’ Compassionate One.
We know well the ravages of computerational malfunction today. Our Desktop had a catastrophic Hard Drive failure two weeks ago, with the backup disc lost. Yikes! Stripes! So, out comes the old Dell D510 laptop. A “gift” from an in-law. A whole 40GB of functionality. Alas! The letter ‘P’ on the keyboard doesn’t work. Now we begin to understand how intrafamilial vendettas get started. All is not lost. A replacement keyboard, easy to replace too, costs only $9.95 USD, shipping free. So, when the next Social Security cheque comes in, I’ll send off for the replacement part. But, there is a sort of a problem. The laptop is running, when it does feel so inclined, otherwise, a pedestrian shuffle, on Windows XP Pro. Hmmm….. No longer supported by the Technarchs. I’m being unpleasantly surprised by how many sites will not ‘hook up’ to an obsolete Operating System. Just getting connected to the Internet in general took me several hours fiddling about yesterday. Luckily, with some reservations about that word, I’m typing this on an old eMachines Desktop I resurrected from the ‘Room of Endless Surprise.’ That had a whopping 160GB Hard Drive capacity, but I managed to slave to it an old Western Digital 250GB hard disc I had picked up for a song in the past. Erase the data on that disc and move the jumper on the connector array and you’re in.
Lest I transgress yet again the “No Chatroom” Rule, I will assert that access to the Internet has become necessary for ‘optimal functionality’ in this society. Many places of “business” now favour Internet communications over all others. The wait queue on a telephonic quest for resolution of one problem or another will make my point, with emphasis. We older ‘folks’ aren’t quite so ‘savvy’ as them young whippersnappers about Internet related ‘things’ in general. Weathering the storms of hardware breakdowns is an additional, mental stressor for the older cohort.
This digression has been to set up our recent experiences with end of life issues as handled, and often mishandled, by the “Medical Industrial Complex: America.” (MICA) As the acronym suggests, the process is populated by and run for the benefit of ‘Flinty Hearted Plutocrats.” Stealing a trope from Lambert, I will assert that the dividing line between the populations headed for ‘Happyville’ or ‘Pain City’ is disposable income. The moment you mention Medicare, you can almost hear mental shutters being drawn down to fend off the offending ‘Poverty Rays.’ It is early days yet in our quest for a user friendly Home Hospice organization, but when you look at the online brochures and blurbs surrounding each potential ‘Savior of the Elderly and Sick,’ do notice the emphasis on happy smiling Servants, and spiffy Pristine Surroundings. I have begun to look each commercial entity up on Indeed and Glassdoor to read the workers comments before I make any further move gathering information. The number of astroturf comments tells me how serious, er desperate, a company is to hide something. The disparaging comments that make particular complaints, versus general ones tells me of particular problems likely to be encountered in engaging that companies services. I particularly have been noticing an almost ‘Underground Theme’ of complaints about management being not only mercenary, but grossly incompetent as well, often both. Often the complaint starts with the information that the company in question has recently been bought by outside interests. I am seeing that as the ‘Kiss of Death’ for businesses in general now, not just healthcare concerns.
Well, it’s time to go into the kitchen and act as Phyl’s “hands” to cook some breakfast. (Due to pain issues, her sleep pattern has become chaotic, to say the least. I often follow along, grumbling and spouting steam like a geriatric geyser.)
See y’all later.
> I have begun to look each commercial entity up on Indeed and Glassdoor to read the workers comments before I make any further move gathering information.
Not a bad item to add to one’s methodology.
Thanks for pulling this together; some of it I knew but the scale and lack of tracking are eye-opening.
When my kids were little, we toddler proofed everything. Now that I am old and living on my own, (a life-saving thing! I control the food that I eat), I am gradually making the house “old person proof”.
I bathe, shower or sauna most days, but I never put soap, detergent or skin product on my skin. I only use soap on my hands or feet if they are dirty. The microbiome on our skin presents a powerful shield against extraneous infections.
Also, I do not eat food with preservatives (natural or unnatural) in them. Preservatives are there to extend the life of the food, not extend our lives. The preservatives/additives mess up the microbiome in our gut. This, again, decreases our defenses against pathogens.
Eat a simple diet. Every other creature, apart from humans, eats one or a handful of different foods.
Sunbathe. The sun is very healing.
I try to focus on staying and being healthy. There is a choice of healthy regimens (Vegan to omnivore to carnivore etc). Generally simple, unprocessed and chemical free.
However, there are an endless number of strategies to be unhealthy. Power and money will not necessarily, make us healthy. The unhealthy wealthy are often kept alive longer………..but only for bilking purposes.
I intend to stay out of “care” for as long as possible. Hopefully, for the duration…
Lambert you are truly the greatest, wish I had more & more time to tell you all the many reasons why… thanks
[lambert blushes modestly]
The impressive Fayetteville Veterans Home appears to be in pretty good shape. Dad’s probably going to be there soon. He’s still in the medical foster care home for now but I talked to the woman there and she sounded tired, dad was wired. Going over there tomorrow with some new slacks and long sleeve shirts I bought for him and my brother said he was frenzied out Sunday.
My dingy brother has taken in another younger person with Alzheimer/dementia, I cannot believe it. Something’s got to give. Was waiting to see what they decide on dad, I’m going back to a twuck dwivin job asap and may never ever come home…
A former colleague of mine died from sepsis a couple of years ago. She was 79 and undergoing treatment for breast cancer. She was a deanlet at an ivy league medical school at the time, and therefore not lacking in disposable income or in VIP status at their affiliated hospital where she was being treated.
Until reading this post I had assumed she died from sepsis because of her age and compromised immune system, but now I wonder.
Trying not to be too jaded, but things are bad in the Mississippi Delta much of the Black Belt, and Appalachia? Hmm, backwaters of the Empire. It has been a long time since the New Deal and the Federal Government investing in these regions. Thanks for rural electrification, roads, dams, and some parks. See you in a hundred years. Check out how many rural hospitals have and will be closing in these areas.
Princeton Medical Center is making an effort to reduce sepsis. Its newsletter says that one of the problems is early detection, as deaths rates rise quickly with delayed diagnosis and treatment. The effort is to make the staff alert to symptoms. It is good protection for the general population to become alert, too. This is a case of a well funded hospital taking preventative action.
Last year I had laparoscopic abdominal surgery in a “world-class” Boston hospital with a two day stay. I turned 60 recently and take very good care of myself (diet, exercise, sleep etc). I walked two miles the day got home and within six weeks was lifting weights, doing 25 mile bike rides and thought all was behind me when very suddenly one morning my temperature shot up over 104 and I began losing consciousness.
After 18 hours in the ER and two days of surgeons denying the possibility of surgical infection, my wife went ballistic (that is what it took) and demanded that Infectious Disease docs be called who ordered MRIs and other scans and within two hours diagnosed me with a surgical/septic infection. I spent the next week in a hospital bed with three IVs in each arm because the Vancomycin and other super-bug antibiotics rot the plastic in IVs and destroy the veins that are used within 24 to 36 hours. It took me far longer to recover from the infection than the surgery.
I am passing on my story to let people know that even under ideal conditions you need to be cautious, weigh the risks of elective-surgery and even entering a hospital for any reason. Most of all, you need to ask questions and advocate for yourself. Doctors are almost always very selective about what information they share and your interest is not necessarily aligned with theirs.
Unfortunately, the vast majority of people do not even have the opportunity to fend for themselves given their need for medical care and little if any real options.
I was on a 10 day backpack 16 years ago, and when I got out of the backcountry, my wife told me my dad had been admitted to the hospital (Kaiser) with a bleeding rectum, and he had Diverticulitis and was an occasional cheater when it came to consuming nuts & seeds, the likely cause.
I saw him 2 days after he’d been admitted, and I knew he was ok, as he was peppering me with how the stock market was faring, etc. We had popcycles together and that was the last time I talked to him, as sepsis set in and he was dead 2 days later.
Interesting article, and thanks for sharing.
Staffing is the reason at both nonprofit and for profit, for profit being a little worse. The nurse is like a floor manager and nursing aids provide the care, up to 30+ patients.
To prevent sores patients need to be turned every 2 hours, diapers cleaned asap when soiled, bath & skin checks done. Feed, clean and dress. Prevent falls.
Many states are moving to get aids medication certified to give the daily meds.
Long term care best avoided.
I found it strange an article about sepsis didn’t mention vitamin C. Getting sick depletes vit c for a reason; try fighting any infection without adequate amounts of C available. Most Americans are vitamin C deficient. (The RDA’s are a joke.) PS: In general, MD’s are the last folks I would go to for advice on Vitamins and supplements. (It’s barely covered in med school, those Drs. who do know anything have learned on their own volition). The reason we are advised to eat multiple servings of fruits and veggies is because of the the antioxidants and other beneficial nutrients present in these foods.
Here’s a recent article about one of many research projects concerning sepsis and Vit C. https://www.npr.org/sections/health-shots/2018/05/11/609149556/can-a-cocktail-of-vitamins-and-steroids-cure-a-major-killer-in-hospitals
Sepsis or ‘blood poisoning’ is probably what most of us die from in the end, the end stage of many debilitating conditions. If infection gets into your blood stream, you are dire straits. The air is a soup of floating microbes and fungi, looking for a nice spot to land–an open sore is an open invitation. So are bottle caps, open bottles, uncovered wounds of any sort, and so on. If you have surgery, try to learn how to do your dressings yourself. Hospital personnel are covered in germs no matter how careful they are.
Old folks, or anyone who can’t move around much, can develop bed sores (skin break down) overnight. Nursing homes have almost no staff, and hospitals don’t seem much better.
I agree. One of the problems is that laparoscopic and robotic surgery are being performed more and more in place of open surgery. There are benefits in this “weekend surgery” but you really need to hunt through the medical literature to understand the significant infection risks and the numbers, in my opinion, the reported numbers are likely far too low because surgeons and hospitals are loathe to acknowledge and report the infections they cause. Instead, they diagnose people who were recently admitted and return with infections as “infection of unknown origin” and pump them full of antibiotics hoping they will get better. Most people also don’t realize that the IV antibiotics used to treat systemic infections these days are horrid chemicals that are extraordinarily destructive to the body. “It’s Like pumping in Drano” is what the phlebotomist/nurse said to me after I asked why the plastic tip was rotting in the IV tube.
@pcraig October 1, 2018 at 2:40 pm
Thank you. Vitamin C was the first thing I thought of when I started reading this.
Also, thanks Lambert, for posting.
Thanks for the article and comments
A relative walked into Memorial Hospital in Florida this summer for a pain, but otherwise in relative good health. She was put under observation on an observation floor. Vital signs started downward 24 hours after admission but nothing done by observation nurses. 32 hours after admission she was in Septic Shock and died next day. When admitted, she had a Lactic Acid level of 4, which as we later discovered is an indicator of sepsis. She was examined by two internists on admission. We later discovered the senior internist and admitting doctor had lied about being currently board certified. They took no action re the Lactic Acid level. No further tests, no antibiotics, nothing. She was around 76. Nurse reminded internist of lactic acid level morning after admission, but senior internist (who was AWOL that day with no covering physician) did nothing, not even ordering another lactic acid test. Only lactic acid test was done on admission. She was on Medicare. Nothing will happen to the hospital or the doctors and this will happen again. Malpractice laws protect hospitals in these types of situation. No apology by hospital.