Yves here. I must confess to not having been sufficiently imaginative. From time to time, we’ve featured posts from Health Care Renewal on the considerable misuse of electronic health records, or EHRs. They offered the promise of much more accurate, consistently documented, and easy to examine patient histories. Instead, they were optimized for billing, not patient care. They’ve become a time sink for doctors and can degrade patient care by forcing the doctor to concentrate on pages of tick the box forms at the expense of examining the case before him.
Here we learn of a new offense: that hospitals are playing definitional games so as to withhold records from patients and the lawyers that represent them, particularly MD notes which can show changes in patient condition versus medical interventions. What is worse, as this post shows, a detailed letter to Mickey Tripathi, the Health and Human Services official responsible for health information technology, got a brush off from a minion.
I encourage concerned readers to write Tripathi and cc their Congresscritters. Merely a short note asking about his lack of interest in this violation of patient rights in the face of HIPAA complaints being ineffective might stir the pot. On issues where bureaucrats expect no one to be watching, it takes surprisingly few letters to get them nervous.
By Informatics MD. Originally published at Health Care Renewal
This exchange I had with the Office of the National Coordinator for Health IT (ONC) at HHS should be of interest. It comes from my now-12-plus years experience as forensic expert in EHR-related litigation:
———————–
April 19, 2023
Micky Tripathi, Ph.D., M.P.P.
National Coordinator for Health Information Technology
Health and Human Services
Washington, DC
Dear Dr. Tripathi,
I am a medical informatics specialist, former Yale NIH postdoctoral fellow 1992-94 and then faculty at the Yale Center for Medical Informatics. I am involved in medico-legal EHR forensics in recent years.
Being involved as an expert in a number of legal matters currently where discovery of electronic records, audit trails and note modifications has been ongoing for up to a decade due to misconceptions, judge confusion, and semantic abuses by the hospital sector has brought me to write to you.
I am writing to you regarding an issue I think ONC needs to comment upon and clarify nationally. The issue concerns EHR information blocking by numerous hospitals and lawyers.
I have experienced many examples where hospitals have arbitrarily defined their “designated record sets” to not include note modifications, and actual note entry times, which in the paper world were an immutable part of the paper record. (The actual entry times were reflected in the note sequence in the paper charts if not written explicitly by authors.) It should be noted that hospitals are taking significant liberties in defining the contents of the DRS so that they mirror the same exceptions of the “legal medical record” when responding to patient requests for their complete medical record.
The hospitals then do not produce note modifications and actual note entry times to patients on electronic record requests, and oftentimes resist requests from their legal representatives. I, in fact, know of a number of cases where this production failure has been ongoing for years, causing significant legal expense in court battles to obtain this information and where justice is thus delayed … or denied.
These actors seem to believe that electronic records reduce patients’ rights to this information compared to patients’ rights with paper records (regarding information that was inseparable from paper records), and that patients and their representatives should be blocked from receiving it in electronic record production.
I think it is self-evident that note changes and modifications in paper records are an immutable part of that paper record and must be produced to patients or the representatives as part of the medical records. Removing, altering or withholding note changes and modifications in paper records would be unquestionably misleading as well as improper spoliation of the records.
In paper records, note corrections through cross-out and user correction/annotation do not turn the original comments into metadata. They remain part of the primary records. Neither do note modifications in electronic records transform the original note into metadata; the modifications remain part of the primary records. Going electronic should not change patient’s rights to this information.
However, in electronic records note changes are usually not shown on the record printout, but only in an audit trail or special report. Hospitals maintain that such record changes including timing of medical record entries are metadata and/or part of an audit trail, and thus not subject to production on ordinary record requests based on their “designated record set” definitions. Production of this information is also often resisted on request of patients’ legal representatives, requiring much legal argument, educating judges on the issues, motions to compel, and wasted time and court resources.
The actual entry order of the notes themselves are also an immutable part of paper records, whereas in electronic records a user-selected display date and time are often used to order the chronologic print out of notes, obscuring the actual sequence of note entry. The actual record times oftentimes are not shown in the standard record printout.
Thus, without the patients’ rights to receive such data with a standard records request, medical care notes and entries can undetectably be entered late – hours, days, weeks or longer after clinical events – and patients and their representatives are misled about when such notes and entries were actually made.
The prevalent standard used by HHS for audit trails in healthcare information systems, ASTM E2147-18, mandates that certified EHRs capture this information – old versions of notes and identity of who changed them and when, and actual times of entry- in their audit trails. But this is being ignored by many healthcare entities in patient record requests.
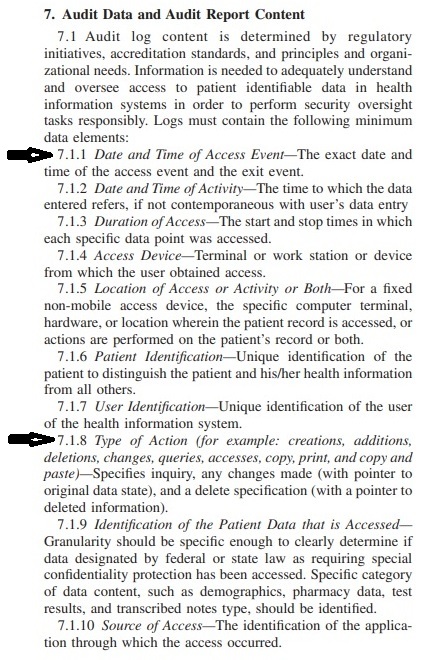
ASTM E2147-18 Audit trail mandatory content (click to enlarge)
My question is this. Does ONC believe that the move to electronic records from paper records reduces patient’s rights to information such as note modifications and note entry times?
If so, why?
If not, a national clarification is needed from ONC to prevent this problem from continuing to occur.
I have also become aware of a member hospital of a larger national hospital chain’s defense team making the following statement about an EMR record where the forensic evidence is undeniable and shows, among other issues, deletion of an important note, but where the defense states to the court that the chart is fine. The case is of a mother whose child was grievously injured at birth. This statement was filed with the court this month:
“… it is this Defendant’s position that the medical records are subject to the business record exception and therefore are authenticated by virtue of the exception.”
This, of course, is a preposterous position regarding authenticity of electronic records, completely ignoring ASTM E2147-18 definitions on authentication and what that entails, but many judges do not know better.
This cannot continue.
Sincerely,
S. Silverstein
—————————————
A response came a few days later:
From: Marchesini, Kathryn (OS/ONC) <Kathryn.Marchesini@hhs.gov>
Date: Mon, Apr 24, 2023 at 3:35 PM
Subject: Re: Letter to ONC DirectorTripathi attached regarding legal issues and EMR information blocking
Cc: Tripathi, Micky (OS/ONC) <Micky.Tripathi@hhs.gov>
Dr. Silverstein:
Thank you for bringing this matter to our attention. From the information you shared with ONC, it seems your questions and concerns relate to the HIPAA Privacy Rule
If you believe that a HIPAA-covered entity or its business associate violated your (or someone else’s) health information privacy rights or committed another violation of the HIPAA Privacy, Security, or Breach Notification Rules, you may file a complaint with the HHS Office for Civil Rights (OCR).
Kind regards,
Kathryn
Kathryn Marchesini, JD, CISSP
Chief Privacy Officer
Office of the National Coordinator for Health IT (ONC)
U.S. Department of Health and Human Services
I responded back:
From: S Silverstein
Date: Tue, Apr 25, 2023 at 12:24 PM
Subject: Re: Letter to ONC DirectorTripathi attached regarding legal issues and EMR information blocking
To: Marchesini, Kathryn (OS/ONC) <Kathryn.Marchesini@hhs.gov>
Cc: Tripathi, Micky (OS/ONC) <Micky.Tripathi@hhs.gov>
Dear Ms Marchesini,
Thank you for your response.
I am aware of the link for filing complaints with the HHS OCR.
The problem I’m describing, however, is a bit different. It is far more pervasive than merely the cases I’ve been involved in, and has a straightforward solution.
What has been ongoing since I started forensics work in 2010 is systematic, ongoing, pervasive discovery abuse and even fraud by a multitude of hospitals and nursing homes in multiple states across this country. My colleagues report the same phenomena.
I’ve personally written dozens of affidavits in the litigation battles for production of complete records, audit trails and note modification histories. I’ve watched delay after delay after delay, wasteful of court resources and money. These battles should be completely unnecessary.
It’s a national problem.
A solution is clarification from ONC and HHS on hospitals obligations for EMR production, that can also educate the judiciary who can be swayed by the most absurd arguments for a healthcare organization’s failure to produce.
For instance, another preposterous claim I’ve heard on numerous occasions in litigation is that the 2010 version of 45 CFR 170.210 did not specifically command hospitals to store or retain note version histories, only user actions. Therefore, prior to the 2012 version (which called for adherence to ASTM E2147), hospitals claim they were given an open license to not store or delete the prior versions of altered notes, turn off that feature in their EHRs, or acquire EHR technology that lacked the capability.
Judges are generally unknowledgeable about these matters.
I hope we can agree that, regarding the 2010 version of 45 CFR 170.210 “Standards for health information technology to protect electronic health information created, maintained, and exchanged”, the stated key issue is:
Protection of health information and electronic medical record integrity.
The 2010 version of 45 CFR 170.210 does not explicitly state that audit trails must contain a note modification history.
However, this regulation could not reasonably be interpreted as overriding paper records standards of care that call for not obscuring or obliterating original versions of altered notes or documents, and giving license to hospitals to capriciously and freely obliterate previous versions of modified notes or documents. That is not protection, that is note destruction.
Such an interpretation is absurd, but is submitted with a straight face in court.
The 2010 version of 170.210 also could not reasonably be interpreted as overriding previous health care information system federal regulations from the very same Dept. of Health and Human Services that regulates hospital electronic medical records systems.
For example in pharma – 21 CFR part 11 of 1997 entitled “Food and Drug Administration, Department of Health and Human Services, ELECTRONIC RECORDS; ELECTRONIC SIGNATURES”, subpart B,
- 11.10 Controls for closed systems,
mandates at (e):
(e) Use of secure, computer-generated, time-stamped audit trails to independently record the date and time of operator entries and actions that create, modify, or delete electronic records. Record changes shall not obscure previously recorded information. Such audit trail documentation shall be retained for a period at least as long as that required for the subject electronic records and shall be available for agency review and copying.
Finally, in 2012 an update to 170.210 did specifically call for electronic medical record audit trails in hospitals to adhere to the ASTM E2147-09 health care audit trail standard of 2009. That standard specifies that in audit trails, pointers must be maintained to previous versions of altered information.
170.210 was later updated to the ASTM E2147-18 2018 version, which about audit trail content says the same as the 2009 version.
Clearly HHS’s intent was to maintain the same standard of care as in paper record keeping, and to not give license to hospitals to obliterate or destroy previous versions of altered notes or documents.
Simple statements from ONC clarifying hospital obligations with regard to production of medical records, note modifications, and other audit data not being optional nor subject to debate, could help resolve the situation that’s ongoing for many years. Discovery resistance is commonly known to EHR forensics specialists and trial lawyers.
The expenses to fight it come from injured patients’ or deceased patients’ family’s potential compensation – that is, when justice is not denied them through manipulation of the EHR discovery process.
Sincerely,
- Silverstein—————————————
I await a further response.
— SS


We have come to the point where it is not crazy for a family to put a nanny cam in a relative’s hospital room, particularly seniors.
Any inquiry into patients’ well-being, hiding malpractice & EHR tampering is now probably a felony & media will soon be bragging about rounding up whistleblowers. I’m unable to find a clear TTE I’d had, between D614.G & my first mRNA-1273 & one showing VITT, after gnarly side-effects?
In English please.
HIPAA is solely to protect commercial transactions, not people. Paper records were not perfect by any means. They could easily be altered in clinics, where access by other providers would be limited. Moreover there were no time stamps of data entry (labs, imaging studies, etc.) where delays or loss (the post office!) could be a plausible excuse.
Unfortunately, doctors also fake physical exam findings, busily running the hamster wheel (in both the electronic and paper world of “protected” health information) to generate RVUs or justify CPT codes. Heart murmur? Decubitus ulcer? Breast lump? No way! A new physical finding.
Telehealth is heavily promoted in this post-Covid 19 era. Actress Kristen Bell is the face of Hers (the grammatically incorrect male product is Hims), marketing pharmaceuticals and OTC products to young women. Like Larry David (who the NYT noted didn’t get crypto and that’s why FTX hired him), Bell doesn’t get the risks of Hers.
Hers and Hims are not covered entities, subject to HIPAA. Check out their privacy policy, with attention to the data collected; and informed consent, with attention to potential risks and data privacy and protection.
https://www.forhers.com/privacy-policy
https://www.forhers.com/telehealth-consent
Also, HHS emergency guidance granting non-compliance for telehealth,is ending soon.
https://www.hhs.gov/hipaa/for-professionals/privacy/guidance/hipaa-audio-telehealth/index.html
“ The Telehealth Notification provides that OCR will exercise its enforcement discretion and will not impose penalties on covered health care providers12 for noncompliance with the requirements of the HIPAA Rules in connection with the good faith provision of telehealth using non-public facing13 audio or video remote communication technologies during the COVID-19 PHE.14 As such, under the Telehealth Notification, covered health care providers can use any available non-public facing remote communication technologies for telehealth, even where those technologies, and the manner in which they are used, may not fully comply with the HIPAA Rules.”
Patient protection is not the goal of our healthcare system. Sleep and eat well. Get outdoors. Meditate. Relax. Garden. Knit. Exercise. Be kind to yourself and others.
“…goal of our healthcare system.”
The US doesn’t have a healthcare system. The US has a profit making system which produces as much profit as possible while producing as little health care as possible as a byproduct.
Paper records set the standard of care for record-keeping, however; the move to computers did not change those standards.
Yet hospitals have taken a stance that patient’s rights to what was immutably part of patient records, such as note alterations and deletions and actual note order of entry/timings, are reduced.
The information has now been mysteriously been anointed to the level of “metadata” (perhaps by the cybernetic Lords of Kobol?), and patients cannot generally obtain this information without an attorney’s help.
Even then, it often is almost as painful as pulling teeth.
We were promised by Obama and all the minions in The New Yorker, NY Times, etc that the EHR would revolutionize the practice of medicine.
Well, the EHR did indeed do that – by converting the medical record into a cash register and turning the entire practice of medicine into an opaque cludge. The blind leading the blind.
1) Back in the day, when I as a PCP sent a patient to a specialist for care, I would universally receive a 2-3 paragraph discussion of the assessment, plans, and any issues they wanted me or my office to take care of. It was on beautiful stationary, written on paper, and there was little if any confusion. I have just looked over my inbox from this AM in an EHR system. I have 27 documents, many of them repetitive because we usually fax things on 3 separate days to make sure they get to the recipient. The least of them was 13 pages long – the greatest was 56. There are pages and pages of gobbledygook. There is no rhyme nor reason to format – so one of them may have important things in the beginning, the next may have them in the middle, the next all over the place. It is an absolute miracle that anything gets done.
2) I am constantly hit up by nagware to upcode this or that document or billing. “Your documentation will allow you to bill a 99214 instead of a 99213, please address”. The documentation is the same as filling out an IRS 1040 on every patient. I am in an office where the previous retired provider never converted to computer records – all on paper. I do have to look through his stuff on occasion – typed out notes. 1-2 paragraphs – I knew instantly what was going on when he saw those patients years ago. Contrasted to today – literally 8 pages of crap for a stubbed toenail.
3) We were promised that all of these systems would communicate with one another. Well, they do not even come close. The level of communicability now is far inferior to the 1980s with fax machines. Again, any attempt to do so from a far off hospital arrives weeks later and is often hundreds of pages of gobbledygook with no ability to turn right to the page, etc. I cannot tell you how many lawsuits I have been consulted where the proximate cause was this exact issue – one small nugget of critical information on page 452 of 1300 pages. Somehow, it is the doctor’s fault for not reading through 1500 pages of documents all the while seeing 20 patients a day.
4) This issue discussed here in this article is alarming. At the core level, the IT people are indeed able to hide and change things. It then becomes a HIPPA violation to reveal the audit codes, etc. What a complete joke
5) The patient portal systems allow instant access to all labs, and tests – CONTEXT FREE. So all the games played – about needing this or that unnecessary test in the documentation scares the crap out of people and we end up doing all kinds of things that are expensive and add nothing to the mix. THIS NEVER HAPPENED before the computers.
6) When you walk onto a hospital ward now, all the nurses are glued to computers. It is as quiet as it can be except for the typing. No colleague to colleague communication at all. Zilch. Contrast to when I was young and I showed up on the wards – there would be a nurse in my face – “IM DOC – get your ass into room 8 – that guy is sick.” Nothing at all like that happens now. Ever. I have seen too much – When it is my turn to get sick one day – I will be doing it at home as much as I can.
7) FYI – there are literally armies of administrative people often dozens a day from the local hospital to the corporate office in another state – going over every aspect of your chart every day. Making sure that every opportunity to bill more or add more services – and to yell at the nurses or doctors to do so – is done multiple times a day. Also, there are AI algorithms in place now that tell the clipboard MBAs when the patient needs to be discharged. Any doctor who dares say a word about keeping people for more days is placed on the path to be DCd at the next available moment when his contract is up.
There is a reason I am encouraging strongly all my own kids, all the young people I teach in Sunday School, and all the kids I have for 4H to do something else but medicine. They need to be plumbers, construction guys, woodworkers, etc. Medicine is just no longer something I would ever encourage any creative, hard-working child to ever pursue.
> When it is my turn to get sick one day – I will be doing it at home as much as I can.
Amen.
And on top of it all, hospital-acquired infections. A torment nexus wherever one looks.
Amen! I gave riddance to my IM/ endocrinology career over two decades ago when I should have been in my prime. Caring for diabetics, I felt like a handmaiden to PhRMA. I knew that was far easier than addressing the social determinants of health. While EHRs were fledgling (and certainly not in outpatient care), the demands to upcode were. So much for the Hippocratic Oath! One has to wonder how medicine will look when the institutional memory of pre-EHR care is gone.
Neither of our kids went into medicine. We’re I young, I would be adrift, baffled about career pathways that could promise a middle class life. I am particularly scornful of people who claim to be serial entrepreneurs. Would Graeber be able to identify any non-bullshit jobs that are rewarded with a living wage, stability and dignity?
I love our vet. She is great at explaining complex information to this layperson, but she is never condescending. She listens, thinks out loud, and gets back promptly with test results. Doesn’t seem burdened by conflicting incentives that bedevil MDs.
If anything is ever seriously wrong with me—so far I’ve enjoyed the robust health that runs in my family—I would really prefer to go to her or, indeed, any of the vets I’ve consulted. I am not the only one I know who feels this way.
“We were promised by Obama and all the minions in The New Yorker, NY Times, etc that the EHR would revolutionize the practice of medicine.”
Ah yes, is that statement about “EHRs WILL REVOLUTIONIZE MEDICINE” one of bellicose grandiosity, or grandiose bellicosity?
See my presentation to the Healthcare Informatics Society of Australia in 2012 for more about “revolutions”.at
https://web.archive.org/web/20170619144902/https://cci.drexel.edu/faculty/ssilverstein/HISA2012_Final.ppt
Revolutions usually turn out badly for a lot of people.
In a different economy, where the first principle is something other than pure profit, an electronic medical records system which is universally reviled by its users would be summarily scrapped. Obviously, that’s not the universe we’re living in.
Otherwise the above post says it all, except that as emr’s go, Epic is by far the worst.
Here was one response. “If you believe that a HIPAA-covered entity or its business associate violated your (or someone else’s) health information privacy rights or committed another violation of the HIPAA Privacy, Security, or Breach Notification Rules, you may file a complaint…..”
It’s right there in black and white. All you need to do is use your criticial-thinking skills to understand what that REALLY means:
“if you believe” — TRANSLATION: you’ll have to hire your own expensive attorney just to see what the Medical Oligarchs and their slavish data collectors have done to revise, skewed or deleted your personal information.
Sending in a “complaint” will do nothing because your live in A Tyranny of Profit Makers who don’t care a whit about YOU!!
I’ve said it before, and I will say it again, the best electronic health record (EHR) created to date is MUMPS, “Massachusetts General Hospital Utility Multi-Programming System”, and that is because it was developed by doctors, not IT types.
It was created in 1967 (!) after doctors as Mass General got sick and tired of the slop served them from IT pioneer BBN.
EHRs are misnomers. They really are electronic billing systems designed to speed reimbursements/payments. Sure, things like bedside medicine verification help, but EBS’ weren’t pushed for patient safety…. They were pushed to get paid quicker with fewer coding errors.
That was Saint Obama’s success story with ACA. The ultimate JV presidency.
This is alarming as well from a malpractice defense standpoint because the records often can help the doctor in a case. But overall the EHR system is nothing more than computerized billing fraud. Putting in physical findings or claims thereof that were not examined is completely fraudulent. And as IM doc points out those multi page reports of chum are filled with word processed crap. And it does hurt patients because often physical findings can help make a diagnosis and can focus treatment efficiently. Otherwise treatment can be based on tests and X Rays without much patient history or physical support. The results speak for themselves. I am struck that I had to see a number of doctors about an ailment recently. Not one even touched me or examined anything. I saw the reports later and they were filled with reports of physical findings. I have no idea how the system can encourage outright fraud as a standard of care. Obviously the pharma med industrial complex is in total control of Washington. If doctors really wanted to change the system and really cared they have a recourse. They could strike and demand a national health care system with all doctors on salary with no fee for service or productivity bonuses. We do not need EHR as IM doc points out. We have way too many specialists all making as much work as they can. America is the dream destination of med school graduates worldwide especially in the third world. We are depriving most of the world health care because their doctors flock to the US to make life altering bank. Half of all surgeries in the US are pointless and do not lead to better outcomes. In spite of all our trillions spent on health care life expectancy is going down. And the usual argument that doctors on salary have no incentive to do a good job is absurd. The lawyers argument that if they cannot sue that medical quality will go down is absurd. A national medical injury fund without lawsuits would make sense. The most critical health care people get is emergency care and that is provided by salaried firemen paramedics and is generally quite good. It is only after the swinging doors of the ER are entered that fee for service for the providers takes over. And a lot of fire departments have discovered the gold mine and now are doing fee for service billing themselves at the 911 level. Doctors could alter this by striking and demanding a federal takeover of health care with everyone on salary. The British NHS is a good model if properly funded. Although doctors could solve this perhaps most American doctors are too far gone to want to put patients before profits. They are paying the price with destruction of the profession.
The NHS is is going down hill and is headed for privatization. It is being purposely destroyed ( as is traditional Medicare in the US.) Since Britain left the EU, US “health” industry are looking forward to make money the American way in Britain.
From a nursing perspective, EHRs drive the care, not the other way around – meaning obvious clinical priorities which address the immediate well being of the patient. Care plans are canned and thus meaningless, repetitious, loaded with jargon, and no longer a usable tool for delivery of care. “Personalizing” means inserting the patient’s first name. Moreover EHRs are time consuming to navigate, time you don’t necessarily have when trying to communicate with another provider or retrieve information in an acute situation or with a change in condition. We gave more effective care with paper charts. That they were designed and purchased by bean counters is another issue altogether.
I’ve wondered for awhile where physicals went! I saw the same GP for the last 4 years and never once did she touch me. Or, apparantly, read my chart. To my astonishment, last time I saw her and complained about my (post mastectomy) arm swelling, she looked startled and said, ‘Did you have a mastectomy?’
I am going to try getting meds online, from now on.
And I bet the computerized physical includes a detailed examination………so that is insurance fraud it seems.