Yves here. The finding in the well-designed, multi-country study below is counterintuitive and very important. Sicker populations show less backing for more generous healthcare provisions than healthier ones. Is it because the extent of ill health raises the specter that a decent level of service translates into more society-wide costs? Or is it a particular manifestation of the general tendency that communities that perceive themselves to have some surplus are more receptive to funding social safety nets?
The authors also highlight the doom loop that seems to be starting in the US: that falling levels of well being translate into less support for broad-based medical programs, which then results in further declines in population-level fitness.
By Marcello Antonini, Visiting Fellow, Health Policy Department London School Of Economics And Political Science; Research Fellow, Centre for Primary Care and Health Services Research Department of Economics, University of Oxford and Joan Costa-i-Font, Professor of Health Economics London School Of Economics And Political Science. Originally published at VoxEU
People’s quality of life is directly affected by policy decisions about access to healthcare and funding, making it increasingly important to understand how the public interprets fairness. This column examines how people’s health status, proxied by exposure to the BCG vaccination, shapes their attitudes towards equal access to care and willingness to pay higher taxes. Individuals with better health are more supportive of fair health financing and equal access to care, suggesting that improving population health may bolster public backing for more equitable health systems.
Fairness in healthcare doesn’t simply mean giving everyone the same resources. In practice, what people view as ‘fair’ is shaped more by shared social norms and ideas of justice than by strict equality (Olsen 2011, Starmans et al. 2017). Most people accept some inequalities when they view the reasons behind them as legitimate, but reject those seen as arbitrary or unjust. Healthcare brings these fairness concerns into sharp focus because decisions about access and funding directly affect quality of life and, in many cases, survival. As health systems face rising costs, understanding how the public interprets fairness becomes increasingly important for policy design.
Healthy or Unhealthy Self-Interest?
A key unresolved question is how personal circumstances – especially one’s own health – shape attitudes toward fair access to care and fair financing of the health system. Evidence from COVID-19 reveals that exposure to the pandemic increased aversion to inequality, especially among those not directly affected by the pandemic (Costa-Font et al. 2021) and affected vaccination, a pro-social behaviour (Voth et al. 2021).
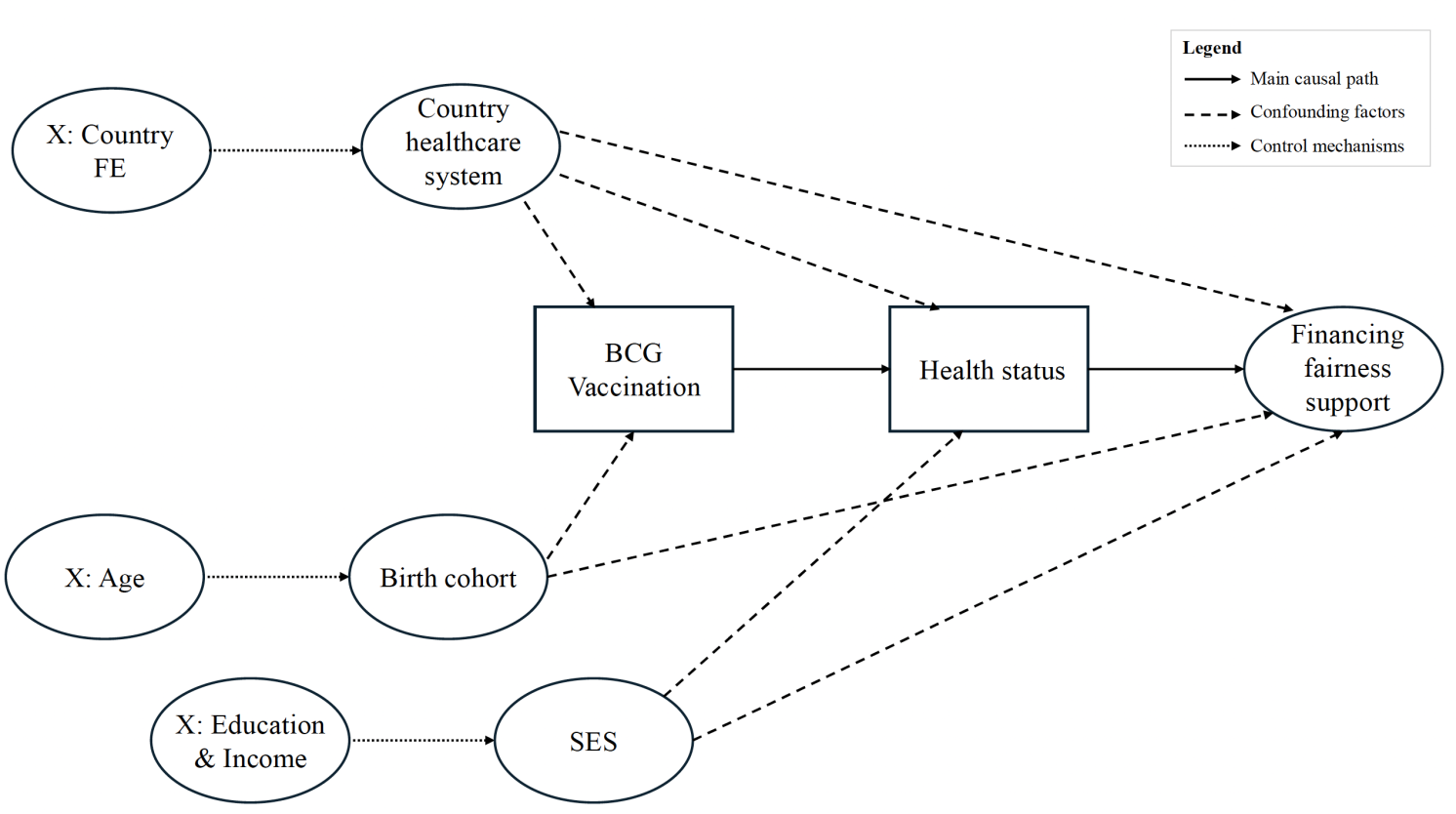
Figure 1 presents a directed acyclic graph that visualises our identification strategy, illustrating the causal pathway from BCG vaccination to health status to preferences for financing fairness, as well as potential confounding factors that our methodology addresses. We consider two competing hypotheses:
- The ‘healthy self-interest’ hypothesis suggests that people in poor health support redistributive policies because they benefit more directly from them, while healthier individuals may prefer approaches based on personal responsibility.
- The ‘unhealthy self-interest’ hypothesis proposes the opposite: that people in poor health narrow their focus to immediate personal needs and therefore show less concern for system-wide fairness, whereas healthier individuals may have more capacity to support fairness norms.
Figure 1 Directed acyclic graph of BCG vaccination instrumental-variable strategy
Health and Attitudes to Health System Fairness
To test for the effect of health-on-health system fairness, in Antonini and Costa-Font (2025) we examine evidence from more than 70,000 respondents in 22 countries, linking self-reported health with attitudes toward equal access and willingness to pay higher taxes for better public healthcare.
Figure 2 illustrates a positive association between exposure to the BCG vaccination and both dimensions of financing fairness preferences. This positive association is particularly pronounced for attitudes toward fair access, which also show higher average scores compared to willingness to support fair financing.
Figure 2 Association between exposure to BCG vaccination and (1) attitudes toward fair access and (2) willingness to support fair financing, at the country level
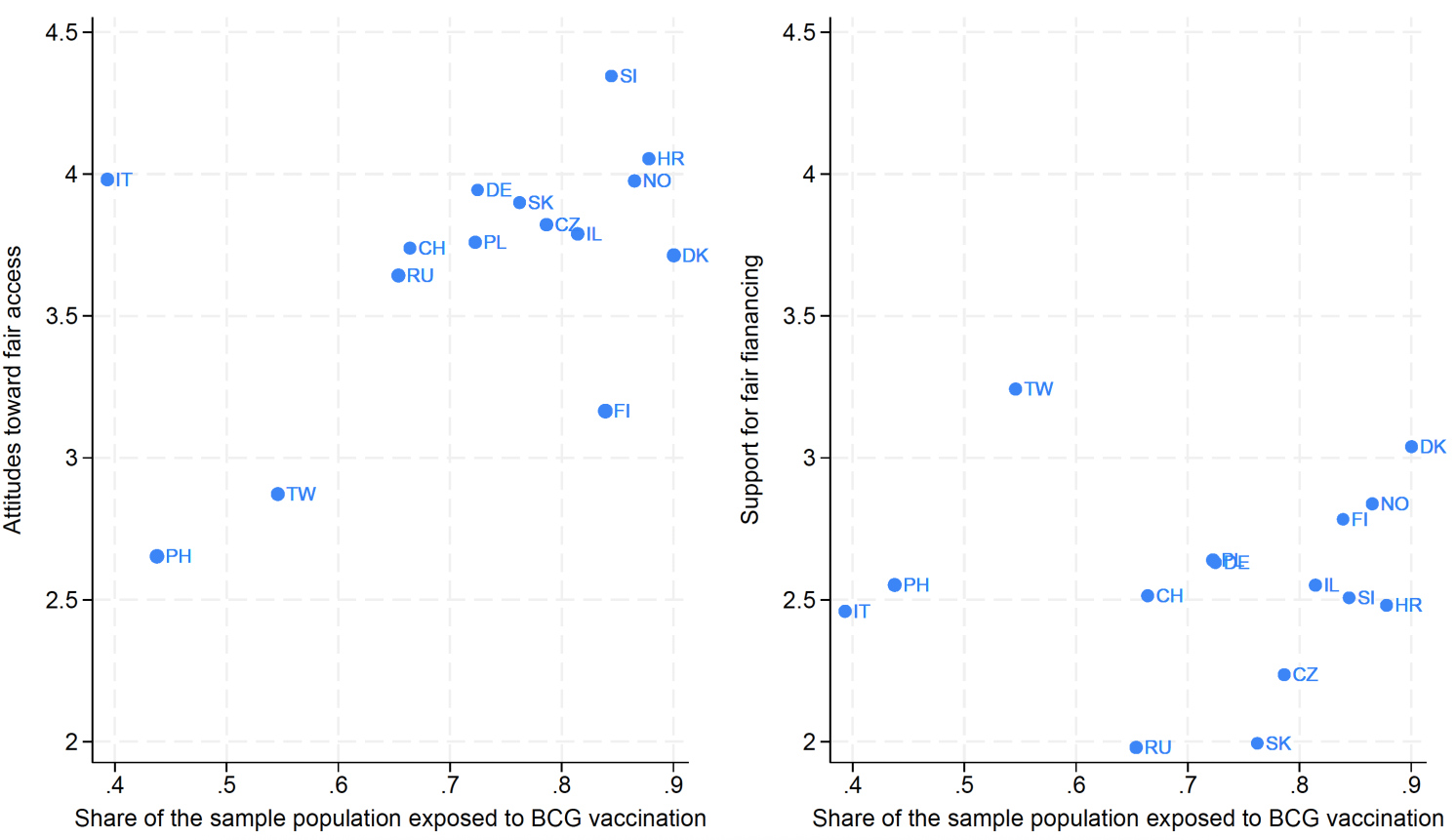
Notes: The figure depicts a scatter plot of the instrument (exposure to BCG vaccination) against the two outcomes of the analysis: attitudes toward fair access (panel 1) and willingness to support fair financing (panel 2), at the country level. The size of the circles reflects the standard deviation of the two outcome variables measured in each country. To create this scatter plot, we first calculated the average concerns for both outcomes for each country. Subsequently, we plot the mean values of the concern variables on the y-axis and the share of the population exposed to BCG vaccination on the x-axis.
The graphical inspection suggests that our instrument may be a valid candidate for the analysis. Our causal estimates are retrieved from a novel instrumental-variable strategy based on variation in BCG vaccination exposure, allowing us to estimate the causal effect of health status on fairness preferences. This approach helps address the long-standing challenge of separating the influence of health from other social or economic factors.
The results clearly support the ‘unhealthy self-interest’ hypothesis. Individuals in worse health were less supportive of fair health financing, while healthier individuals showed stronger support for both equal access and more redistributive funding. A one-point improvement in self-reported health increased support for fair access by 11% and support for fair financing by 8%. These findings suggest that improving population health may not only enhance wellbeing but also bolster public backing for more equitable health systems.
Our findings suggest a stronger effect on normative judgements compared to behavioural intentions involving personal costs, suggesting that health status has a more pronounced impact when no personal financial sacrifice is required. This pattern indicates that while healthier individuals express greater support for fairness principles, this support somewhat diminishes when it involves actual financial contribution.
The mechanisms driving these effects operate primarily through economic pathways (income and employment), with healthcare trust and political attitudes playing contributing roles. This helps explain why healthier individuals, who typically have better economic outcomes, demonstrate greater preferences for fairness in healthcare financing.
These findings also help explain why more unequal societies often experience poorer health outcomes such as lower life expectancy, higher obesity rates, greater substance abuse, and worse mental health. When people experience ill-health, their support for fairness in healthcare access and financing weakens, making it less likely that policies aimed at improving equity will gain traction. Notably, this pattern appears across very different healthcare systems, suggesting that the link between personal health and support for financing fairness is universal, even if its strength varies by institutional context.
The causal connection between better health and stronger support for fair healthcare financing points to a potential virtuous cycle. As health systems succeed in improving population health, public backing for equitable policies may naturally increase. This dynamic may help explain why health inequalities sometimes follow a Kuznets-type curve (Costa-Font et al. 2018). It also reinforces the case for investing in health improvements as a foundation for long-term equity. As overall health rises, systems may be better positioned to apply fairness-oriented allocation tools – such as fairness weights – and to prioritise historically overlooked groups whose needs become more visible.
See original post for references


This seems like a special case of the general rule that the better something works, the more effort and resources one can give, knowing that they won’t be wasted. So, an unresponsive policial system produces abstainers and low information voters. Apparently, health care works the same way.
A case of the chinken or egg first question?
“This helps explain why healthier individuals, who typically have better economic outcomes, demonstrate greater preferences for fairness in healthcare financing.”
“prioritise historically overlooked groups whose needs become more visible”
“people in poor health narrow their focus to immediate personal needs and therefore show less concern for system-wide fairness”
maybe
historically overlooked groups have tended to be the poor, discriminated against, socialy outcast and economically ‘disadvantaged'(the poors and the others). This disadvantage creates a constant stress – an induced survival mode with definite negative health consequences. Anotherwords, this explains why ‘disadvantaged (poor) people’ generally have unhealthy outcomes whose needs have historically been ignored and are to busy with basic survival to be concerned with a concept of “system-wide fairness” for which they have never been included.
Just my uninformed opinion for which I offer no offense
Yes, you are unto something here…From my neck of the woods I can clearly and loudly claim that the cause-effect relation starts with poverty leading to bad health outcomes. And it starts before one is born. Materially and socially deprived women deliver premature and underweight newborns in a higher proportion than better off women. And it continues. Early development indicators are strongly correlated with material and social deprivation.
Thus, poverty is the latent variable that explains a lot when it comes to health outcomes. And these poorer people, when they are asked about a more social healthcare system, imagine that the cost will be on them, and they already are in the negative. Maybe if the question would have been whether or not they think that the taxation for healthcare should be progressive, the more you have, the more you have to give would have elicited a different response?
Having done such large survey research in the past it’s remarkable how difficult and nuanced interpretation of such data can be. And how many biases can be introduced at all levels. Beyond just those that are an intrinsic part of such policy oriented data gathering efforts. Then adding the multicultural international aspect of this…
In the US, having grown up in a ‘traditionally’ underserved community I think people are aware they are sicker and don’t get all the healthcare (including quality nutrition and environmental conditions) that they need. But they have been bombarded from birth by two juxtaposed messages.
First, America has the best healthcare in the world and everyone else wishes they had it.
Second, our stellar healthcare is necessarily the most expensive in the world and doing even a little more would drive the costs TO THEM exponentially higher.
People don’t see these things in isolation. And here ‘those people’ attitudes are prominent.
“Even if I pay more I won’t get more, or better. The rich will always get better and when they say equity it just means more going to those people and not me and mine”
“They’ll just raise the drug prices and nothing will change”
“My doctor is good. It’s those insurance companies that will take any extra.” (The sicker people are I think the more desperately they want to believe THEIR doctor is good.)
“Raising my taxes won’t do anything about the industrial plant down the road that’s giving us all cancer”
Healthcare isn’t like buying a sofa.
Now project that onto 22 different nations with different reasons for participating and their own ways of choosing who to interview and how. And asking some very broad questions. I’m well aware of what NORC’s ‘quirks’ were in the 80’s. I can only imagine the situation elsewhere.
I’d definitely look on this as interesting but tenuous.
This looks to me to be more of what Wilkinson and Pickett explained in The Spirit Level: Why Equality Is Better For Everyone
https://www.penguinrandomhouse.ca/books/395860/the-spirit-level-new-edition-by-richard-wilkinsonkate-pickett/9780241954294
I find the analysis in this study unconvincing due to potential confounding between key variables and age.
For example, BCG exposure is purely defined as a function of age within each polity. Anyone born while the polity has an active BCG campaign, regardless of actual uptake , is considered exposed. Its inclusion basically marks out the oldest individuals, with the specific cutoff varying by the historical development of the polity in question, and the youngest individuals in the case of more developed countries. That there is an association between such a crude covariate and health status speaks more to the non-linear effect of age on health than the more specific interpretation the study advocates.
You can actually see the issue at scale in Figure 1. Three late implementers of BCG campaigns (Italy, Philippines, and Taiwan) have high leverage (i.e. the extremeness of their dependent variable values gives them great influence over the estimated correlation). If you cover these up with your hands, the apparent effect essentially disappears.
Experience tells us that both health status and political leaning are associated with age. So one alternative interpretation is that younger people, who are much healthier (beyond the linear effect already modeled) also tend to be more supportive of fair access to healthcare.And this is just one of the potential confounders, with income being another (which is itself confounded with age).
Moreover, the analysis, as presented above, groups the respondents by country. Maybe there is additional analysis in the original research paper? The important thing would be to compare the poorer and less healthy people to the richer and healthier ones *within* a country, since they share the same health care “system” (as flawed and unequal as it may be) and the same spectrum of political opinion and propaganda. To do it by country and compare across countries, to my mind, can only conclude that countries where the support for financing health care is low have poor average health – which is the chicken and which is the egg?
Indeed, the effect of the country was modeled as country-specific constants added to individuals in the respective country. It’s still a spherical cow model, since the comparative development trajectories were anything but parallel when First, Second, and Third World (in the original sense, too) states are all represented in the dataset, but it’s not as fatally flawed as the graphical analysis (why did they even include it?) suggests.