By Lambert Strether of Corrente.
Patient readers, I apologize for being late; I got the bright idea of checking the masking policies of the hospitals with which HICPAC members are affiliated late in composition, and although it does nail the post’s thesis, it took longer than I expected.
Let’s get the engineering stuff out of the way first, because masking is too important to be left to the medical community. Covid is airborne (a.k.a. aerosol transmission); people infect each other with Covid via “shared air”, which floats like cigarette smoke. Covid is airborne in hospital settings. Masks work to prevent airborne transmission[1].
Infection control guidance for hospitals that deviates from these engineering principles costs patients’ lives. It really is that simple.
As readers know, I have long railed against the hospital infection control community for its tooth-and-nail resistance to the “engineering stuff” summarized above. CDC’s HICPAC (Healthcare Infection Control Practices Advisory Committee) is providing a fine example of massive resistance that, in another context, would have made George Wallace proud[1]. CDC describes HICPAC and its putative mission as follows:
HICPAC is a federal advisory committee appointed to provide advice and guidance to DHHS and CDC regarding the practice of infection control and strategies for surveillance, prevention, and control of healthcare-associated infections, antimicrobial resistance and related events in United States healthcare settings.
Here is HICPAC’s structure, from CDC’s About page:
HICPAC consists of 14 voting members who are not federal employees. These experts are appointed by the Secretary of HHS following an application and nomination process. HICPAC voting members bring expertise including, but not limited to, infectious diseases, infection prevention and control, healthcare epidemiology, nursing, clinical and environmental microbiology, surgery, hospital medicine, internal medicine, epidemiology, health policy, health services research, public health, and related medical fields.
HICPAC also includes six ex officio members who represent federal agencies within HHS, as well as liaison representatives that bring related patient safety expertise from health-related associations, consumer groups, public organizations, and partners. These ex officio members and liaison representatives are included on the HICPAC charter, which is renewed biennially by HHS. Ex officio and liaison representatives are non-voting members of HICPAC.
“Related medical fields” is doing a lot of work there. Since airborne transmission and its prevention are fundamentally engineering problems, some might find it surprising — given that #CovidIsAirborne — that there are no aerosol sciencists or ventilation engineers on the Committee. Then again, if we view HICPAC as the highest expression of the Infection Control hive mind, we might not find it so surprising.
HICPAC is currently reviewing CDC’s guidance on masks and infection control generally, and has already done a lot a lot of damage to patient (and health care worker) safety:
We testified today at a closed door meeting where @CDCgov HICPAC Commitee recommended that #N95s are no longer needed to prevent #COVID19 transmission, although #COVIDisAirborne
The presenter wore a KN95 while sharing a flawed collection of mask studies #HICPACUndemocratic 🧵 pic.twitter.com/XA2dAwa408— People's CDC (@PeoplesCDC) June 8, 2023
The next meeting is August 22:
#KeepMasksInHealthcare Folks, this is the meeting where it really matters: pic.twitter.com/xWH0eYtcdp
— Mary Ray (@MaryRay555) July 3, 2023
There’s nothing now on CDC’s site describing the upcoming HICPAC meeting’s agenda, or when, or how to register, but the Daily Beast (of all sources) has this to say:
HICPAC will meet in August and may vote on proposed updated guidelines for infection control—and it may end up exacerbating concerns rather than assuaging them. An informational slide deck outlining the committee’s proposed updated guidelines, obtained and reviewed by The Daily Beast, makes little mention of aerosol transmission of viruses, and cites what experts say are flawed studies to suggest there is no difference in the protection offered between respirators like N95s and surgical masks.
If accepted, the guidelines could enshrine unsafe practices for health-care workers at a time when the industry is already suffering from critical staffing shortages.
In the section discussing pathogen transmission, there is only a cursory mention of aerosols and airborne transmission, but no real discussion of the types of protection needed for different types of viruses. More shocking, however, is the Evidence Review at the end of the slide deck, in which the studies cited by HICPAC as supporting evidence of its conclusions do not appear to be as robust and persuasive as many public health experts expected.
In a later post, I’ll examine HICPAC’s guidelines more closely. In this post, however, I will examine the Committee itself. Personnel, after all, is policy! Here is the roster of HICPAC members:
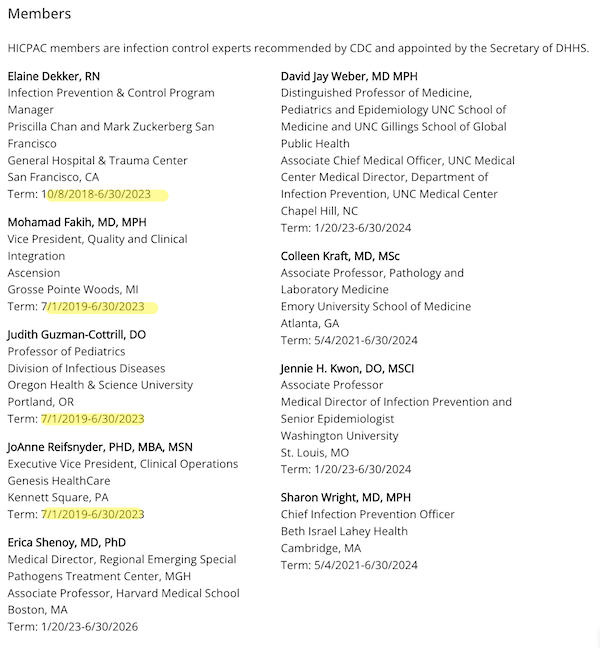
(I have highlighted the members whose terms are said to have expired; but since there’s no new roster, I must assume that their terms have been extended somehow.)
I will now go through each committee member, present any relevant publications, and present the current masking policy of each hospital with which they are affiliated. (Unsurprisingly, they are all following CDC’s guidance MR SUBLIMINAL Because CDC is following their guidance, but it’s good to get that on the record. We are, after all, looking at a symposium of infection control titans; it would be surprising indeed if not one institution still implemented universal masking. Or perhaps not so surprising.) I’m going to examine the members a little out of order, because I notice an old friend–
Erica Shenoy, MD, PhD. Shenoy is, of course, one of the authors of this infamous article, reviewed at NC here. I can’t give all the detail, but will quote the essential note [A]:
Here is the key paragraph for Shenoy’s second claim. Since this is yellow wader-level, er, material, I’m going to add some letterered notes, thus “[A]”:
Maintaining masking requirements for [Health Care Personnel (HCP)] during all direct clinical encounters[A] may marginally reduce[B] the risk for transmission from HCP to patient or from patient to HCP. Those potential[C] incremental benefits, however, need to be weighed against increasingly recognized[D] costs. Masking impedes communication, a barrier that is distributed unequally across patient populations, such as those for whom English is not their preferred language and those who are hard-of-hearing and rely on lip reading and other nonverbal cues[E]. The increase in listening effort required when masks are used in clinical encounters is associated with increased cognitive load for patients and clinicians (5)[F]. Masks obscure facial expression; contribute to feelings of isolation; and negatively impact human connection, trust, and perception of empathy (6,[G] 7[H]).
Before going further, I should point out that today masking by staff is common in Asian hospital settings. Therefore, all of Shenoy’s claims are negated for almost half of humanity. If I were so-minded, I’d call out Shenoy for being Eurocentric, or colonialist, or even racist. To the detail–
[A] Shenoy — it seems hardly possible — seems not to recognize that Covid is airborne, spreads like smoke, and is present everywhere, not merely in “direct clinical encounters”; that’s why masking needs to be universal throughout the facility.
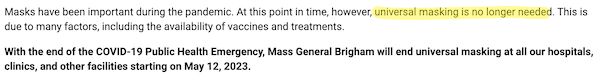
Shenoy is affiliated with Mass General Brigham. Here is their masking policy:
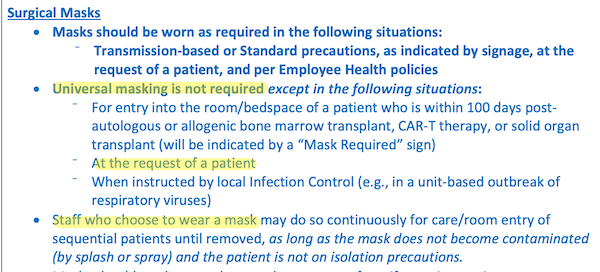
Sharon Wright, MD, MPH. Sharon Wright is a co-author of Shenoy’s vile screed (and I’m not exaggerating). Wright is affiliated with Beth Israel Lahey Health. Here is their masking policy:
Elaine Dekker, RN. Here are Dekker’s views on masking on April 8, 2020:
We asked Infection Control Director, Elaine Dekker what she does to protect herself. Elaine rides the 9 Muni every day to and from her home in the Tenderloin. Up until last week Elaine did not wear a mask and she continues to not wear gloves. Here are her tips.
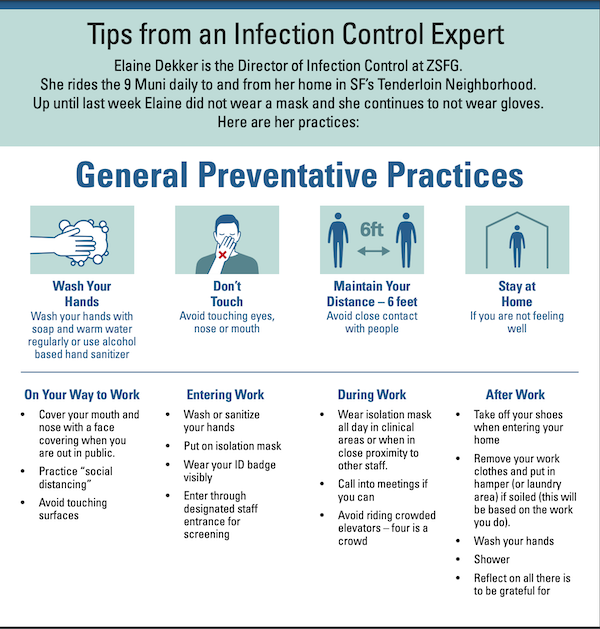
One cannot, I suppose, blame even an infection control maven for focusing on fomites and droplet dogma (“6 foot distance,” “close contact”) even in April 2020. I suppose.
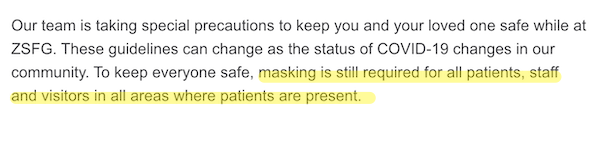
Dekker is affiliated with Zuckerberg San Francisco General. Here is their masking policy:
Mohamad Fakih, MD, MPH. Here is a letter from Fakih in Infection Control & Hospital Epidemiology, June 2020:
In times of stress, people also assess their ability to cope with the threat (ie, coping appraisal). Thus, the motivation to engage in protective behavior is heightened with the belief that the recommended protective measures would lead to successful outcomes (ie, response efficacy) and when there is confidence in one’s ability to perform healthy behaviors (ie, self-efficacy; for example, “I am able to constantly perform hand hygiene and mask.”)
Once again, I suppose it’s OK to believe that handwashing prevents Covid transmission in June 2020. I suppose.
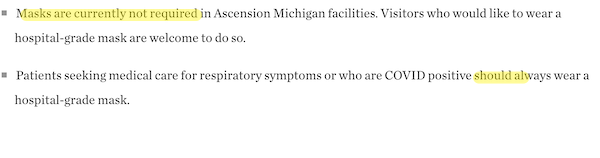
Fakih is affiliated with the Ascension hospital chain at their Grosse Point, MI facility. Here is their masking policy:
Judith Guzman-Cottrill, DO. Here is one article of which she is a co-author, from July 2022:
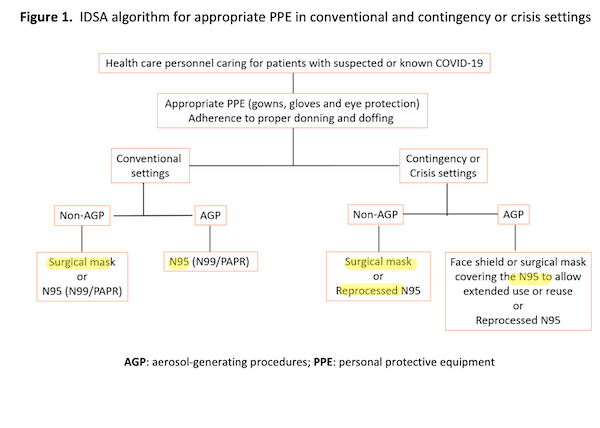
I’m kinda shaking my head at the complexity of this tree structure (and every node has a rent, a concept I shall return to) but at least every leaf (highlighted) recommends a mask of some sort!
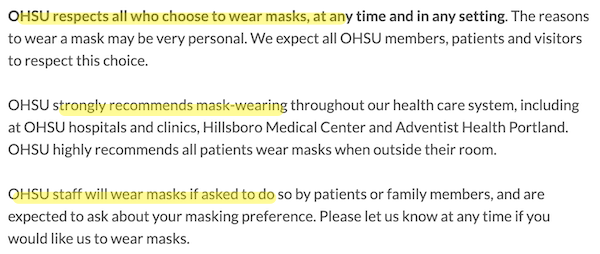
Guzman-Cottrill is affiliated with Doernbecher Children’s Hospital. Here is their masking policy:
JoAnne Reifsnyder, PHD, MBA, MSN. Reifsnyder is affiliated with Genesis, an enormous nursing home chain. I can’t find a Genesis mask policy, or relevant publications from Reifsnyder.
David Jay Weber, MD MPH. Here is a 2023 article for which Weber is a co-author:
One of the lessons learned during the COVID-19 pandemic wasthe important role ventilation plays in the transmission of the virusin healthcare setting. The outbreaks reported among staff, patients,and visitors to the healthcare facility highlighted that attentionneeds to be given to adequate air flow and correct directional flow.The World Health Organization guidance on addressing theinadequacy was a timely help for many during the crisis. There is an urgent call for all healthcare institutions to review the ventilation in all areas, even for daily patient care, because it is fundamental to ensure adequate ventilation to prevent healthcare-associated infections associated with common respiratory viral pathogens such as influenza, respiratory syncytial virus, etc. This review work is best conducted in consultation with the facility engineers and IPC professionals as a team. Inappropriate design of the healthcare facility may often be a root cause for inadequate ventilation. Although there may be specifications for the design in some developed countries, these may be absent in low- and middle-income countries. Nevertheless, it would be expected that a healthcare facility be designed to facilitate safe patient care [lol no].
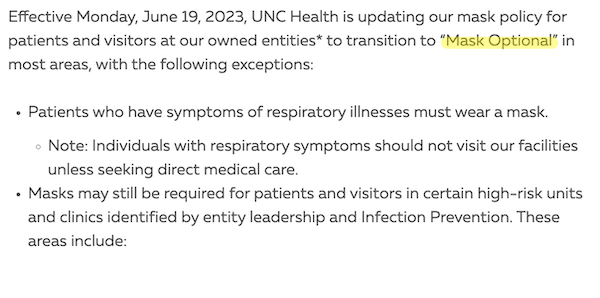
Weber is, at least, sound on ventilation. Weber is affiliated with the University of North Carolina. Here is their masking policy:
Colleen Kraft, MD, MSc. Here Kraft expresses her views on CDC’s 2021 mask guidance:
“So we know the Delta variant can’t get through masks, and so we need to go back to the things that worked, even though we were hoping with increasing uptake in vaccination that people could kind of be able to do their normal activities,” she said.
One question raised during the press conference was whether the U.S. has put too much faith in the vaccinations, especially since states have been unable to increase vaccination rates.
“I think that we needed to put our faith in something,” Kraft said. “I do think that if we had achieved sort of a high vaccination rate, we would have felt that we had been able to stop transmission before the delta variant could have gotten into our borders or come from our borders, whichever way it was transmitted.”
Kraft seems relatively sound on masks (“they work”) but interestingly seems to believe that vaccines halt transmission. Kraft is affiliated with the Children’s Hospital of Los Angeles. Here is their masking policy:
Jennie H. Kwon, DO, MSCI. Here is a 2023 article for which Kwon is a co-author:
Overall, 86% of DHCP [Dental Health Care Personnel] reported having prior training. DHCP increased the use of PPE during COVID-19, specifically N95 respirators and face shields. DHCP reported real-world challenges to applying infection control methods, often resulting in PPE modification and reuse. DHCP reported double masking and sterilization methods to extend N95 respirator use. Additional challenges to PPE included shortages, comfort or discomfort, and compatibility with specialty dental equipment. DHCP found the educational video helpful and relevant to clinical practice. Fewer than half of DHCP reported exposure to a similar video.
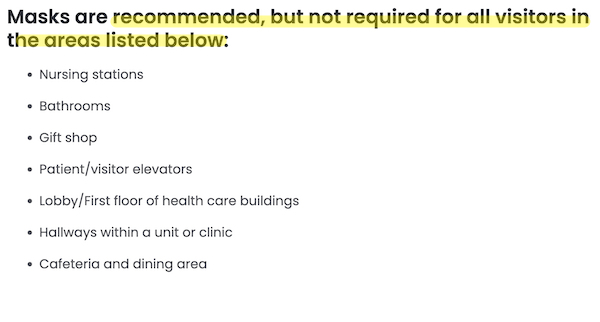
Interestingly, Kwon seems to be the only HICPAC member involved in improving mask uptake and effectivness. Kwon is affiliated with Barnes-Jewish Hospital. Here is their masking policy:
1. None of the hospitals with which the HICPAC members are affiliated have a policy of universal masking.
2. Though some of the HICPAC members look not unfavorably on masking, and on airborne transmission generally, none could be characterized as advocates.
3. Favorability toward universal masking, ideally with N95s, is inversely correlated with institutional clout; Mass General/Brighams vehemently opposed; the University of North Carolina and Barnes-Jewish persuadable.
4. The HICPAC committee members are in the pleasant position of being able to ratify as guidance policies that their institutions have already adopted (i.e., no universal masking, let along universal masking with N95s, going forward). One might, indeed, go so far as to characterize the HICPAC meeting as theatre, were there drama involved in a clearly pre-determined outcome[2].
I would, nevertheless, try to join the August 22 teleconference. There’s nothing wrong with throwing a tomato at a rotten performance!
NOTES
[1] Or maybe the context is the same. Covid infection, after all, disprotionately affects BIPOC.
[2] Going even further, one might characterize HICPAC as thoroughly conflicted.


I think you should reconsider.
My impression is that you remain personally fearful of Covid and that is clouding your analytic lens. I don’t know your health history, this might be justified. Or not.
My suspicion is that you’ve anchored your perception of risk to the early pandemic, not the current era where >96% of the population has some immunity, either through vaccination or previous infection. (1)
I also suspect that in addition to the effect of underlying health, e.g. age, comorbidities (2), there are genetic variations in how susceptible individuals are to bad COVID outcomes, whether it is related to their MHC allele (3) or their vitamin D polymorphism (4). And that, to put it bluntly, the most vulnerable have already been selected out. Hence the risk to survivors is quite a bit lower.
I also subscribe to the virulence-transmission hypothesis, e.g., that a pathogen will gradually become less virulent over time. Though I admit that in the case of COVID this remains to be seen. (5)
In any event, on a societal level, both weekly hospitalizations (6) and weekly deaths (7) are at an all time low.
Finally, this has to be considered in the context of the very weak evidence in favor of masks. While there is a biologically plausible mechanism, e.g., COVID is airborne, high quality masks filter the particles. The reality is that the history of medical reversal is littered with things that seemed like a good idea at the time, but collapsed under scrutiny.
So what do the data say, the Cochrane Review states “wearing N95/P2 respirators probably makes little to no difference” in catching flu like or respiratory diseases. Particularly when objective measures, e.g. laboratory tests, are used to confirm infection. (8) They do clearly admit that the studies are of low to moderate quality. And like them, if better data are forthcoming, I will reconsider.
In this setting public health authorities have to make a decision. How long do we impose a cost (forced mask wearing) on a population for a very limited, perhaps unmeasurable, benefit? Particularly when imposing this cost imposes its own second order costs on the system as a whole? (e.g., increased political conflict, decreased credibility of public health, perhaps decreased responsiveness to future public health measures)
I would argue that the costs of mandatory masking greatly outweigh the benefits and that it is irresponsible and unethical to mandate anything in the absence of data to support it.
You may have a different opinion. That is your right, but I think you should update your priors. And, not to put too fine a point on it, you should consider whether your tribal affiliation is interfering with your analysis.
If you persist, then you should make a falsfiable prediction as to what will happen if they go ahead and relax mask requirements. Mine is that this winter’s peak of COVID hospitalizations will not exceed 22,000 and that weekly deaths will not exceed 1,500. Both less than half of last winter’s peak.
(1) https://www.cdc.gov/mmwr/volumes/72/wr/mm7222a3.htm?s_cid=mm7222a3_w
(2) https://www.nature.com/articles/s41598-023-29364-8
(3) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9867832/
(4) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9953304/
(5) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10066022/
(6) https://covid.cdc.gov/covid-data-tracker/#trends_weeklyhospitaladmissions_select_00
(7) https://covid.cdc.gov/covid-data-tracker/#trends_weeklydeaths_select_00
(8) https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD006207.pub6/full
For the record, I am a physician. I’ve been in hundreds of rooms with COVID patients. My hospital was hit so hard we ran out of room in the morgue and were stacking bodies in the bathroom until we got a refrigeration truck. I am fully vaccinated and boosted. Never got COVID. I still wear an N95 when I see patients, mostly to simplify things for them, but also to reduce the risk of exposing them in case I have an asymptomatic infection. I don’t insist on masks and I don’t wear a mask any place else.
> Cochrane
Come here often? (and I’m not the only one with this view).
Your ad hom deserves, or at least requires, a more detailed response, but unfortunately for the readers I am pressed temporally. Perhaps later. Adding, I’m sure your patients are grateful for your service, as am I. Sadly, the Covid discourse is littered with well-credentialed MDs who, to be frank, know nothing outside the boundaries of their practice, including transmission and epidemiology, and whose views endanger patients, despite their clinical success.
No, I don’t come here that often anymore. I used to about 10 years ago. Was looking for Yves to post a link about Mckinsey.
Not an ad hom because I’m not attacking you. I assume, based on reading you intermittently over the years, that you are operating in good faith. I’m sincerely trying to get you to reconsider your opinion. That includes reassessing your cognitive biases. We all have them. Yours are pretty plainly visible. Because I respect you, I tried to make it as fact based as possible.
I, like you, am not an epidemiologist. I do have publications in immunology, however. I’m also a professional consumer of the medical literature.
Thanks for the link, I just read your previous post about the Cochrane study. I think you don’t appreciate the importance of RCTs or for that matter, what Cochrane does and why it is important, both socially and from a statistical standpoint.
One of the things I had to learn in making the transition from scientist to actual practicing physican was clinical humility. Our reductionist models of physiology, biochemistry, immunology etc, do not always map cleanly onto complex organisms, much less heterogenous populations. Curing cancer in a T75 flask is easy, curing immortal tumor lines implanted into an inbred mouse model is more challenging but do-able, but curing actual humans with actual cancers is a completely different story. Things that sound good on paper don’t always work out in real life.
That is why we have RCTs. While there are certainly things that are not amenable to RCTs, jumping out of a plane with or without a parachute is the classic. That’s not the question here. It’s more akin to asking does mandating every passenger airline have parachutes for all the passengers save lives?
In other words, the question is not, does a brand new N95 mask block particles greater than 0.3 microns. It’s does mandating masks reduce Covid transmission in a population over time. Will it reduce hospitalizations. Will it save lives?
After looking at the best available evidece in the most rigorous way possible, the answer is probably not.
Clinical ethics then requires me not to advise, much less compel people to accept an intervention without an evidence base.
If you recall, this was the position of Fauci and the rest of the establishment before the pandemic panic took hold. No evidence to support masks.
Again, I encourage you to put aside your ego, re-examine your biases and consider the possibility that the people who do this for a living, e.g. HICPAC, though flawed humans, know what they are doing and are attempting to use the best possible evidence to act in the public interest rather than to advance their secret QAnon or WEF agenda, then look at the data yourself and see if there is anything that supports compulsory masking in the current setting.
If you decide that you couldn’t be less wrong, then make a prediction for peak weekly hospitalizations and deaths this winter and I will come back in February and we can discuss.
> Not an ad hom because I’m not attacking you.
> Again, I encourage you to put aside your ego
Dude.
No time to engage in Gish Gallop with you just now, I’m afraid. So sorry. Hopefully I’m be able to review the current literature with you shortly, especially on [genuflects] RCTs.
Of all places the precautionary principle should be a key foundation in healthcare – where the most vulnerable and by definition patients are high risk typically because they’re in a hospital. And that’s what this topic is about – healthcare.
I wrote a long good faith reply, but lost it when my computer froze, so I will cut to the chase… if you truly believe that relaxing mask guidelines is going to be harmful then please make a prediction of just how bad the long winter of severe illness and death is going to get.
Peak weekly hospitalizations due to Covid:
Peak weekly deaths due to Covid:
That is an assignment and a violation of our written site Policies. You are accumulating troll points.
Really? In all seriousness, you think I’m trolling?
All three of my posts were made in good faith as evidenced by the effort I put into them. I spent about an hour writing the first post and and I sourced everything to studies I’ve actually read in their entirety, not just the abstract. I read his post on the Cochrane study and my reply addressed his discounting of RCTs. My third post initially addressed some of the other comments that were directed at me (and physicians in general) but I lost it, so I tried to pick up the thread of the discussion.
I would argue that rather than trolling, I’m making an evidence based challenge to his interpretation. I’m not attempting to mock him, not trying to derail the conversation.
Upon reading the policies, I admit that asking him to make an estimate on peak weekly infections/deaths counts as an assignment and hence a violation. However, I would argue that it was justified.
First because this is a scientific topic and it is a core scientific principle to demand that someone who advances a theory make falsifiable predictions upon which that theory can be evaluated. Otherwise, you’re in the realm of metaphysics.
Second, I would say that asking someone to make a prediction is a useful rhetorical device because it forces them to clarify the implications of their argument, in this case if you want to argue in favor of an intervention you should enumerate and justify the cost benefit ratio.
Finally, I think it’s actually more considerate to let someone state their own case rather than put words in their mouth. I have no idea what Lambert thinks apart from what he has written. Presumably he thinks that removing the mask mandate is going to make things measurably worse, but maybe I’m wrong. Maybe he objects to it on principle, e.g., involuntary exposure of patients to risk. Maybe he thinks it’s going to cause a catastrophic return to the bad days of COVID or maybe he thinks the effect will be slight, but doesn’t want to go there because even one excess death is one too many.
In sum, I am not a troll. I made a direct good faith argument regarding an intervention on which I have an informed professional opinion and have a personal stake in the outcome, since I and my patients are subjects of said intervention.
Oh, please. The wounded PMC posturing and protestation that effort = good faith. Horseshit. For starters, propaganda and artful distortions take effort too. And more specifically, Lambert and I have moderated over 2 million comments. Trolls often put considerable effort into making themselves heard.
You started with an unforgivable and (inherently) unsubstaniable personal attack on Lambert. That ALONE is grounds for banning as a blatant attempt to bias readers against Lambert on his core beat and denigrate the Covid-careful.
And then you have the nerve to try to insult Lambert’s and the readership’s intelligence after such a flagrant personal attack of trying to claim you did no such thing. That level of fabrication we call Making Shit Up and is separately grounds for banning.
In fact, your opening salvo is projection, accusing another of emotional bias when you are the one apparently suffering from it. The evidence is overwhelming that every case of Covid does damage (as confirmed in brain scans) and repeat infections result in compounding harm. Anyone who isn’t taking precautions is bad at math and risk analysis. But you clearly have an ego investment in having your environment confirm that you carrying on as if Covid were over is a sound choice.
Oh, and the fact that you managed to be one of the first comments when making a smear is also a sign (but admittedly not proof) of trolldom. We see this regularly on hot topics, that we put up a post at say 2 AM with a pro-union position and the first comment is from a union-hostile newbie. We can’t prove it but it sure looks like they had a Google alert on key words in the post and are paid or self-appointed enforcers.
You have no right to expect, let alone demand, a personal response to your nastiness. We bloggers put our work into posts and any participation in comments is if we damned well feel like it.
You follow your personal attack with what Lambert correctly labels as a Gish gallop, yet another bad faith strategy.
And then in yet more bad faith you concede you violated our Policies but double down and insist you have a right to. My God, the sense of entitlement.
Sorry, this is my private hosted space and your whinging is a waste of my and moderators’ precious time.
So yes, you are a troll. You’ve engaged in multiple flavors of trollish behavior. Time to look in a mirror, buddy.
I trust you will find your happiness on the Internet. Elsewhere.
“In this setting public health authorities have to make a decision. How long do we impose a cost (forced mask wearing) on a population for a very limited, perhaps unmeasurable, benefit? Particularly when imposing this cost imposes its own second order costs on the system as a whole? (e.g., increased political conflict, decreased credibility of public health, perhaps decreased responsiveness to future public health measures)”
I’m going to redress your comment just on this one paragraph, Duh.
A. Public Health authorities you say, gutted and IP pro corporatist flexian revolving door appointee thingy you mean. Sorry, saying Public these days is a bit wobbly at best.
B. What’s the inference about – imposed a cost – ***forced mask wearing*** and a completely unscientific opinion about unmeasuable benefit, mask regardless of any environment protect the wearer full stop and that is the science.
C. Now your going economic about costs on the system, ill defined, near or far term, what is the next quarter report all that matters and the effects down the road are – ????
D. Wrapping your argument around the notion of Public Health in America is a massive joke as Corporations have shown complete disregard for it so a few make huge pay days ….
It’s the worst sort of gaslighting as it’s presented as considered dialog …. how do people like you live with yourselves ….
Thank you Dr Duh for providing an insight into the mindset of physicians.
When healthcare workers do not follow hand hygiene protocols, asking them to grasp the implications of aerosol transmission is expecting far too much from them.
One of many studies with the same conclusion about physician behaviour:
Overall, the involved ICUs showed low levels of adherence to best hygiene practices. This suggests the need to implement immediate strategies for infection control in the ICUs. A multidisciplinary intervention could be effective in preventing and control the HAI [Healthcare Acquired Infections] risk.score was reached only by the third year students with regard to the proper HH. The level of knowledge about HAI was inadequate.
…
Although “zero risk” cannot be achieved in ICUs, the infection risk can be easily assessed with simple instruments and efficaciously managed by implementing adequate protocols and procedures to increase quality of care. The results of our research suggest that even if HH [hand hygiene] is still the main action line in reducing infection risk, its importance is not yet well known among the studied ICUs staff.
Prev Med Hyg. 2017 Sep; 58(3): E231–E237.
PMCID: PMC5668933
PMID: 29123370
Disease transmission will be reduced by engineering measures. Expecting healthcare workers to change their behaviour is entirely unrealistic, as your comment demonstrates.
I do like how Lambert’s all “¡¡Engineering Data!!” and gets “You seem fearful.”
Mocking people as fearful is a tactic of the anti-vax movement – and no they don’t see the irony. They call it “mental illness” because they think mental illness is an insult.
Oh, they can be made to change behavior, particularly in a world of corporatized medicine. Put out cameras and dock pay for poor compliance. It’s not hard at all. It just requires enforcement.
Thanks, Dr. Duh! Appreciate your lengthy post. I’m with you on this, as an elderly person myself.
Seems like some people have lost their minds with excessive Covid fear. There are dangers but we need to keep them in perspective and in balance. Masking forever is s TERRIBLE idea.
You too need to read our site Policies:
Using notions like “lost their minds” is just waffle ….
BTW there is nothing to fear[tm] from covid as its not some person hunting you and wanting to take your freedoms away[tm]. Its just a virus that has no concept of humanity or what its doing and just does its evolution regardless of all that.
Ignore that on your own personal level and cop the consequences is fine with me, but, suggesting others should follow your perspective is another thing.
You would really be better served if you had a read of the history of infectious diseases, winging it does not cut it.
PS covid does not care about what rolls around in your head.
> PS covid does not care about what rolls around in your head.
Not to be critical, but I would have said “sloshes,” rather than “rolls.” #JustSaying.
> some people have lost their minds with excessive Covid fear
Rational apprehension of Covid is adaptive. That’s why we have reason, and why we have that particular emotion.
Repeated Covid reinfection is maladaptive, as many, many studies have shown.
Of course, this will take some time to play out. The mills of Darwin grind slowly, but they grind exceedingly small (and indeed there will be time to hand out Darwin Awards to the coterie of bent, know-nothing medicos who should stay have stayed in their lanes, instead of encouraging innocents to engage in behaviors potentially deadly to others and themselves; cf. Luke — the beloved physican — at 17.2).
I shouldn’t be shocked by an elderly person who hasn’t figured out that masking, and hand washing, are minimal long term measures that protect them. I am, but I shouldn’t be. I also shouldn’t be amazed that anyone who must have seen the deterioration in healthcare provided by our “greatest healthcare system in the world” would believe that the faux non profit and outright for profit doctors’ practices and hospitals are going to install expensive engineering systems to make up for inadequate hygiene practices. Just remember all those improved ventilation systems we saw being installed…or didn’t.
Masking, proper masking, should be being demanded by every person on Medicare and Medicaid, everyone with asthma, everyone with children, because it isn’t just Covid, it is RSA, there is even an upsurge in TB. All of which will have decreased transmission with masking.
I don’t think anyone can argue about hand washing.
Just remember every time you avoid infection your life expectancy doesn’t get whacked. Or I guess you don’t know any body who went to the hospital for something minor and got sicker.
Adding, I should have said “clinical success, if any,” since, to be fair, you made no such claim, at least “for the record.” My bad.
The Cochrane review you cite is such egregious and obvious charlatanism that it amounts to self-indictment by the authors.
Your own contribution here comes suprisingly close to being as bad. What is your field?
In a recent Clinical Update by Dr. Daniel Griffin, he stated that we are currently on track to reach 80K Covid deaths this year. It is his belief that eighty to ninety percent of those deaths are preventable.
We may have great individual health care providers and wonderful medical technology but that does not obviate the fact that we have a medical system that adds up to considerably less than the sum of its parts. Our public health policy as concerns Covid has surrendered, not to the necessities of essential economic activity, but to the forces of profit driven commerce.
> Griffin
He doesn’t give his source or methodology. I’m sure deaths are greatly down, but I’m not sure how much I trust the precise numbers. WHO’s numbers were garbage, not even updated. CDC authored the “Green Map,” so…
So, you need more data to support the benefits of (universal) masking, despite the simple physics and biology involved, but don’t need any data to demonstrate the severity of costs and second-order costs of “forced mask wearing”. Surely you see the cognitive dissonance at play? Your post reminds me of the many meteorologists and other scientists in the ’90s and ’00s who insisted that climatologists warning of imminent climate catastrophe were irresponsible to argue for a cessation of fossil-fuel burning — the costs and second-order costs of shifting our energetic economy required more data before limits could be imposed. That these meteorologists, atmospheric physicists, and chemists were terribly wrong does not, of course, imply that you yourself are wrong. However, like you, these scientists’ obstinate demands for “more data”, paired with their relative societal power (‘surely my favorite local weather man must know what he’s talking about?’), has contributed to delaying our economy’s transition away from fossil fuels, guaranteeing tremendous costs, first-, second-, … n-ordered to society, civilization, and much of the rest of the living world. Please consider the damage your own cognitive dissonance may be inflicting upon your community. You have power; please use it responsibly, even it it involves humbly staring the obvious in the face.
Good gravy man do you believe the tobacco industry PR too? – facepalm –
Looks like the HICPAC members were mostly hand-picked as they could be counted on with coming up with the ‘correct’ solutions going by the examples talked about here. It is noteworthy that this will be a teleconference because then the people will be able to show their smiles. But whatever conclusions they come up with, this will what will filter down to hospitals and health practices with the justification of ‘following the science’. I wonder how many of them were signatories to the Great Barrington declaration come to think of it. There were over 16,000 medical and public health scientists who marked their name on it so the odds would be good.
> I wonder how many of them were signatories to the Great Barrington declaration come to think of it.
That’s a very good question. My guess is few to none, but for tribal (“ZOMG, MAGA”) rather than medical, let alone ethical or moral, reasons.
Forgive me for asking. But where are these places that “force masking” ?
Here in my little corner of the upper mid-west, few healthcare workers in hospitals or clinics wear a mask.
People who do wear them are elderly, and/or sickly looking. Does the sight of someone wearing a mask for their own health upset those who can’t be bothered?
Right now the quarrel is over whether venues that provide healthcare services, hospitals in particular, should require masking.
The actual reason for the conflict is that infectious disease control is as financially corrupted and morally bankrupt as economics. In fact my impression is that moneyed interests’ subversion of the field predates them getting serious about economics.
Erica Shenoy can go kiss the bricks at the PR clown version of Indy because she’s racing to win
https://medium.com/@watermelonpunch.com/erica-shenoy-can-read-my-lips-i-dont-want-to-risk-my-health-family-to-see-her-face-b08952c75462
Does she advocate getting rid of mosquito nets where malaria is endemic? what a joker.
I haven’t ever commented on all the masking stuff on NC to date, but it’s a reason I come to the site less often. Totally unconvinced that you are right or that there is sufficient evidence for masking.
And I’m in my 70’s and absolutely hate masking in medical settings (fortunately I rarely see doctors). It majorly increases my stress and ability to communicate.
I am SO MUCH HAPPIER in everyday life now that most people don’t mask and I can see people’s faces. The harms of masking are NOT trivial or inconsequential.
Hi
I like your comments that include being open about your state of anxiety. Good to discuss perhaps. I’m 73 BTW and am still quite COVID-19 aware.
I holidayed in Japan for 4 weeks and returned a week ago. I experience anxiety about COVID and situations that to me are risky. I liked being in Japan because it had strong masking with what appeared to be *all* people-facing workers wearing a mask. And many many others wear a mask too. The ‘Asian’ question is interesting – visually and culturally a visitor, visual takes are guesses(?) and maybe a bit racist. Non Asians (visually!) often didn’t wear masks. I did. People that look ‘Asian’ and that didn’t wear a mask – I wondered if they were visitors?
Air conditioning is plentiful – I assume it’s infection free air. I’m totally in support of the aerosol engineers and want them to design my environment! Closed-in crowded unventilated spaces are anxiety creating. Masks don’t make me feel anxious, they reduce anxiety.
Aotearoa (New Zealand) has masking in the health services I use. I can’t remember seeing a barber wearing a mask (they cut men’s hair). Masks are rarely worn outside of healthcare. Natural ventilation is cold at times though can feel plentifully used (the New Zealand way? :) ) Government does not seem to run public health campaigns on COVID-19 any longer. Overall, the changes here can lead to many more opportunities for me to feel anxious. I forget to mask up sometimes – I’m brought down to reality with a bump.
I recommend Japan as opportunity-rich in lessening anxiety – If I were to stay longer I’d develop a strategy perhaps for avoiding non Japanese people. Non mask wearers get to seem brazen in their lack of care.
Thanks!
People don’t like lots of things. I don’t like taking pills, or getting surgery either. But I like dying a lot less. So as a grown up with the ability to think rationally and overcome emotional hurdles, I do what needs doing for the health of myself and others.